Abstracts
Abstract
The purpose of this article is twofold. First, the study addresses questions related to the spread and impact of the 1918 influenza pandemic in a small Newfoundland community, focusing on the role of large social institutions including an orphanage, school, and churches. Records indicate, for example, that residents of the orphanage in St. Anthony, our study community, experienced an increased risk of infection at different times during the epidemic than did members of the general community. Further, archival sources show that a variety of public health measures including closure of public gathering spaces were implemented throughout Newfoundland, but evidence suggests that the success of these measures varied. Second, this paper presents an argument for the important role computer simulation models can play in historical research, which is demonstrated using results from simulations focusing on social, demographic, and cultural factors, including behaviours and interactions of community residents. These examples highlight how modelling techniques can be used in historical research to address gaps in archival sources and help direct future research paths, and to test counterfactual scenarios to identify important factors influencing observed outcomes.
Résumé
L’objectif du présent article est double. D’une part, il traite de questions liées à la propagation et à l’incidence de la pandémie de grippe de 1918 dans une petite collectivité de Terre-Neuve. Il s’attarde au rôle des grandes institutions sociales, y compris l’orphelinat, l’école et les églises. Des sources indiquent, par exemple, que les résidents de l’orphelinat de St. Anthony, agglomération à l’étude, ont été exposés à des risques plus grands que les membres de la collectivité en général à divers moments de l’épidémie. Qui plus est, les archives révèlent que différentes mesures de santé publique, y compris la fermeture des lieux de rassemblement, ont été mises en oeuvre dans tout Terre-Neuve, mais des données suggèrent que ces mesures n’ont pas connu le même succès partout. D’autre part, l’article soutient l’importance des modèles de simulation informatisés pour la recherche en histoire. Pour ce faire, il utilise les résultats de simulations articulées autour de facteurs sociaux, démographiques et culturels, y compris le comportement des résidents de la collectivité et leurs interactions. Ces exemples mettent en lumière comment les techniques de modélisation servent à la recherche en histoire pour combler les lacunes des sources archivistiques et orienter les recherches futures ainsi que pour tester des scénarios contrefactuels afin de dégager des facteurs importants qui agissent sur les résultats observés.
Article body
Although the impact of past infectious disease epidemics and pandemics (worldwide epidemics) has long been an interest of historians,[1] present-day concerns regarding emerging and re-emerging infectious diseases, bioterrorism, and the potential for rapid global spread of disease have spurred new research on historical epidemics, particularly the 1918 influenza pandemic. Like most infectious disease epidemics, the 1918 flu influenced and was influenced by numerous political, economic, geographic, social, and cultural factors. These factors operate at multiple levels ranging from individual and local to institutional and global. Historical analyses have led to better understanding of the context surrounding epidemics, resulting in a richness of insights that extend far beyond the statistical analyses of morbidity and mortality data that are common methods used by epidemiologists.
The study of historical epidemics presents an opportunity to engage in another increasingly popular research trend, the application of computer simulation models. As modelling software and digitized records become more available, historians must consider the current and future role of technology in preservation, collection, analysis, and interpretation of archival and other data. In a recent essay, John Bonnett[2] observes that “historians don’t like computers much” as he encourages colleagues to instead embrace computing approaches in their research and education activities. Effectively using computer applications provides benefits such as improved critical evaluation of sources and handling gaps in primary source data. These and other benefits of computer modelling have become increasingly recognized in many disciplines, including fields interested in historical and contemporary epidemics. In particular, computer simulation has been used to enhance understanding of how complex factors interact and contribute to systemic processes and observed outcomes.
In order for a computer simulation to be useful, however, both its overall structure and the values chosen for model parameters must be grounded in reality. When dealing with past epidemics, this knowledge can only come from analysis of ethnographic and archival materials. Thus, an essential first step in the development of a computer model for an historical event is an analysis of available archival data that inform about the nature of the population and events being modelled. Once a suitably grounded model has been developed and tested, it can then be used to supplement other types of historical methods in the evaluation and assessment of specific factors identified as potential explanations for outcomes observed in the historic record.
We present here an illustration of how historical analysis is used in the design of a computer simulation of the spread of the 1918 influenza pandemic in a small community on the island of Newfoundland and how, in turn, results of model simulations help us understand the real and potential impacts of the pandemic on the study community. We first provide a brief overview of findings from archival, ethnographic, and historical sources on the characteristics of both the pandemic and early twentieth-century Newfoundland and Labrador that were used to build the model, followed by a description of the model itself. We then show how the model can be used to address two specific questions related to the role of social institutions on the spread of the disease: 1) the potential influence of an orphanage in the study community on epidemic patterns of spread, and 2) the impact of public health measures, including the closing of public gathering places, that were implemented in different communities within the Dominion in an attempt to control the spread of the pandemic.
The 1918 Influenza Pandemic
The 1918 influenza pandemic resulted in as many as 50–100 million deaths worldwide, including about 55,000 Canadians and 675,000 Americans.[3] A recent comprehensive study estimated total worldwide mortality to be 2.5–5.0 deaths per 1,000 people.[4] However, mortality during the pandemic varied widely, with very few deaths in some locations compared to over 90 percent mortality in other affected areas, as was the case in some isolated villages in Labrador and Alaska.[5]
The pandemic generally occurred in three waves. The first broadly recognized wave occurred in the spring and summer of 1918 and was relatively mild, resulting in many cases but relatively few deaths. The majority of deaths occurred during the more severe second wave, which began in autumn 1918. The third global wave took place in early 1919 and was also mild. Some areas also experienced a small “echo” wave in 1920, while outbreaks of a flu-like illness in 1916 and 1917 may have been early cases.[6]
Many factors contributed to the worldwide spread of the pandemic. One major influence on global spread was troop movement and related activities during World War I.[7] For example, Mark Osborne Humphries[8] has demonstrated that the introduction and spread of the disease in Canada was a direct consequence of the war effort, even at the expense of public health concerns. Contrary to previous views that the pandemic was brought home by returning soldiers, evidence suggests it was actually brought in by soldiers from the United States on the way to Europe and then disseminated westward by the mobilization of the Siberian Expeditionary Force. At a more local level, factors contributing to the spread of disease likely included demographic characteristics and daily activities of the population, as well as access to health care and other resources. Public health interventions varied and included closing schools and churches, prohibiting public events, the compulsory wearing of masks, quarantines, and vaccines which, considering the exact cause of influenza was unknown at the time, were of questionable value.[9] These interventions varied in effectiveness and rates of compliance or enforcement; in many cases, they failed to stop the spread of disease.
A well-known characteristic of the pandemic was its W-shaped age-specific mortality pattern. During typical seasonal epidemics, mortality rates are highest in the very young and very old age classes, producing a U-shaped mortality curve. These age groups were still most likely to die during the 1918 flu, but death rates among young adults were higher than typically expected.[10] Outcomes also varied with other characteristics of affected individuals, including proximity to urban areas, access to health care, sex, and preexisting conditions such as tuberculosis.[11]
Research into the pandemic by Canadian historians has exemplified what Howard Phillips[12] termed “second-wave” historiography of the 1918 flu, focusing on social factors such as gender and class to provide a deeper, multidisciplinary understanding of the complex factors and outcomes of the disease. For example, some researchers have examined the role of the pandemic on the development of city and provincial public health departments,[13] while others have considered the impact of the pandemic, as well as the war and other catastrophic events, on the legitimization of the nursing profession, often by analyzing gender-related images and perceptions of the traditionally female occupation.[14] Additionally, historians have challenged the claim that the disease was equally likely to affect all members of society by exploring the disproportionate burden, in terms of morbidity, mortality, and consequences such as loss of wages or costs of funerals, suffered by more vulnerable populations, including First Nations communities, immigrants, and members of lower socioeconomic status, in Canadian experiences of the pandemic.[15] In their recent edited collection, Magda Fahrni and Esylllt W. Jones[16] bring together research that addresses similar questions about social and cultural impacts of the pandemic across Canada, and in their introduction they highlight areas where additional research is needed, such as environmental studies.[17] Although Newfoundland and Labrador was not part of Canada at the time of the pandemic, it was linked to its future country in many ways, e.g., socially, economically, and geographically. The work presented here contributes to the understanding of the pandemic’s influence on the development and history of Canada by investigating the disease experience in a region relatively understudied in Canadian historiography of the pandemic.
The Flu in Newfoundland and Labrador
Newfoundland and Labrador, then an independent dominion within the British Commonwealth, was hit hard by the pandemic, with the highest mortality rates occurring among Labrador populations.[18] Provincial records list 1,885 deaths from influenza, pneumonia, and/or related causes during the pandemic on the island of Newfoundland, giving an average mortality rate of about 74.5 per 10,000 people. At the district level, mortality rates were highly variable, ranging from 28.6 to 109.3 deaths per 10,000 people. Proximity to resources in more populated areas may partially explain this variation, as case fatality rate estimates are lowest in the Avalon Peninsula near St. John’s and increase the farther away the district is from the capital city.[19]
Like other areas around the world, the island of Newfoundland experienced three waves of influenza, although they occurred generally later than the global waves noted by most researchers. Mortality records indicate the first, mild wave lasted from approximately 1 May to 31 July 1918. The second wave occurred approximately 10 September 1918 to 5 June 1919. It was bimodal and severe, with the majority of the deaths occurring during this period. The third wave was again rather mild and did not reach the island until the spring of 1920.[20]
Newfoundland and Labrador government and business leaders employed numerous measures in attempts to reduce or stop the pandemic. For example, advertisements in 1919 warned that individuals recently recovered from the flu would not be cleared by doctors to join sealing crews.[21] However, these efforts were typically concentrated in St. John’s and were variably enforced. For instance, although ships with sick sailors were quarantined in St. John’s, no official actions were taken to hinder regular shipping activities.[22] Additionally, while newspaper notices indicated that all places of public gathering should be closed, correspondence with the Colonial Secretary’s office clarified that these notices were only applicable to the city of St. John’s, and magistrates in other communities were responsible for issuing similar orders if illness struck.[23] At least one community, Greenspond (in Bonavista Bay), reported that “Advent services were all lost” to the pandemic, though it is unclear if this loss was a result of proactive or preventive closure, or required cancellation, or low attendance due to illness.[24] Generally speaking, it is unclear from the historic record how consistently public health interventions were implemented and followed across Newfoundland, especially outside of St. John’s, or how successful these actions were in mitigating the pandemic’s impact.
Life in Early Twentieth-Century Newfoundland
The computer simulation described below is based on a detailed understanding of the structure of Newfoundland communities and the daily patterns of social interaction in these communities. In this section, we describe essential features that have informed model structures.
By the time of the pandemic, the population of Newfoundland and Labrador was about 255,000 people. About 4,000 people lived in Labrador, and about 40 percent of the remainder lived in or near St. John’s. The rest of the population was mostly distributed among small villages along the coast, known as outports, which were geographically isolated and often were home to only a small number of families.[25]
This settlement pattern reflected the economic and subsistence emphasis on marine resources, which also influenced organizational patterns observed within outports, especially prior to the 1949 Confederation with Canada. Fishing crews were small and typically consisted of fathers, sons, and brothers; thus, families tended to settle patrilocally.[26] Families usually lived in nuclear households, although young couples and their offspring often lived with the husband’s parents for some time after marriage before relocating to independent dwellings nearby.[27]
Families shared in labour and responsibilities, with women and children frequently assisting in shore crews processing catches, and most family members contributed to household income in some ways. Women’s activities in shore crews and other areas were estimated to bring in at least half of the family income.[28] Ethnographic and historical literature also highlight the importance of visiting among households and involvement in community and service organizations. In general, multiple sources suggest residents in small outports were highly connected, somewhat egalitarian, and organized strongly around kinship, crew, and institutions such as churches.[29]
During the first half of the twentieth century, the economic base, level of social services, and general conditions of health in Newfoundland and Labrador were much poorer than those of contemporaneous countries elsewhere in Western Europe and North America.[30] Outside of the Avalon Peninsula in the eastern part of the island, where St. John’s is located, roads and railroads were nearly nonexistent, except in the immediate vicinity of larger towns (Figure 1). High levels of poverty were omnipresent, with about one-third of the population dependent on public relief,[31] and there was a lack of running water in St. John’s and many outports until well into the 1960s.[32] The majority of deaths were attributed to infectious diseases until the second half of the twentieth century. Tuberculosis was a particular problem; rates in the Dominion in 1939 were higher than “any other portion of the British Empire inhabited by white people”.[33] Nutritional deficiencies were also a chronic problem until the mid-twentieth century.[34] Even in the mid-1940s, it was common for rural residents to have no food available at winter’s end other than black tea, homemade bread, and jam or molasses.[35] Medical facilities were also inadequate in the St. John’s region and poor to non-existent elsewhere (other than our study community of St. Anthony — see below).
Figure 1
Map of Newfoundland showing location of roads, railroads, and district boundaries (district names in all capital letters) on the island in 1949. Note St. Anthony at the tip of the Northern Peninsula and St. John’s on the northeastern edge of the Avalon Peninsula.
Nonetheless, throughout the first half of the twentieth century, the government and local volunteers repeatedly implemented measures designed to improve the health and welfare of the residents, including construction of hospitals and clinics, better training of nurses, education programs for mothers, improvements in sanitation and sewer services, and expansion of efforts towards tuberculosis control.[36] Owing to the overall low socioeconomic base of the Dominion, however, truly significant improvements did not take full hold until after Confederation with Canada in 1949.
The Study Community: St. Anthony
The computer simulation used in this research is designed to approximate a single Newfoundland outport at the time of the 1918 influenza pandemic. The community of St. Anthony (Figure 1) was chosen for this purpose. The community was large enough to include individuals of all ages and a variety of different occupations, but small enough that sufficient runs of the simulation can be done in a manageable amount of time. In order to make the model population realistic, specific demographic characteristics of the agents, such as age, sex, and occupation, were taken from the 1921 census listing for St. Anthony,[37] which indicates a community of 503 individuals, distributed into 84 dwellings and an orphanage.
A second reason for the choice of St. Anthony as the study community is that it was the home base of Wilfred Grenfell, a British doctor who, in the early 1890s, founded a prominent medical mission, the Grenfell Mission (later the International Grenfell Association). The mission provided health care and other services to residents of northern Newfoundland and parts of Labrador, and continues to do so today. The mission constructed several hospitals in Labrador as well as a hospital and an orphanage in St. Anthony, and recruited doctors and nurses primarily from the United States and the United Kingdom to serve the community and other outports. These doctors and nurses spent their summers on ships that travelled along the coasts of Labrador and northern Newfoundland providing health care to the thousands of fishermen that came to the area from all over the world. Medical personnel who stayed in the region after the fishing season continued to provide health care during the harsh winters.[38] As a charitable organization, the International Grenfell Association kept detailed records of their activities, including a local journal, Among the Deep Sea Fishers, that was published quarterly from 1903 to 1981.[39] Information from these and other archival sources were used to develop realistic scenarios of daily life in the simulations.
Although Newfoundland and Labrador as a whole was hit very hard by the 1918 pandemic, archival sources suggest that the town of St. Anthony largely escaped the second and most severe wave. Hospital records indicate that, while 26 people were treated at the hospital throughout the epidemic and eight patients died, only about one-third of these cases occurred during the second wave. In addition, the first wave cases were residents of nearly a dozen different communities who travelled to the hospital for treatment, suggesting that the outbreak was widespread in the region.[40] Influenza was definitely present during the second wave, however; an outbreak occurred in the St. Anthony orphanage where records indicate that 34 of the 37 children fell ill and one died.[41]
It is not clear why St. Anthony (and the Northern Peninsula in general) escaped the severe second wave that ravaged most of the rest of the island. Analyses have focused on the role of prior immunity, a stoppage in regular boat traffic because of flu further south, and possible interactions between influenza and one or more other pathogens, but a definitive answer has not been forthcoming.[42] It is also difficult to determine why the orphan children were affected so severely during the second wave, given the likely widespread prevalence of influenza in the St. Anthony region during the first wave. Entrance dates for orphan children indicate the vast majority had been admitted prior to the first wave, making it unlikely both that these children escaped prior exposure to the flu during the first wave and that the outbreak was due to the introduction of the disease by a newly orphaned child.[43] We illustrate below how our model may help to shed light on how these patterns may have arisen.
The St. Anthony Computer Simulation Model
To test hypotheses related to the spread of the pandemic in St. Anthony and similar communities, a computer simulation model has been developed. Models, in a broad sense, provide frameworks for identifying essential components of a system or process under study and can be used to explore how variation in those components affects outcomes. Agent-based models are being used more commonly to create this kind of framework. Such models explicitly consider a system or process within or produced by a group of discrete units or agents (e.g., individual organisms, households, or communities). These models often include stochasticity (randomness) and can incorporate as much data as desired, such as population movements, climate data, or geographic coordinates. Thus, agent-based models tend to be complex and computationally expensive to simulate compared to other types of models.
Though the use of simulation is not common among historians, calls for increased use of these methods have intensified over the past quarter-century.[44] Currently, historical simulations are most common in the realm of military history, where war games are formalized into Monte Carlo simulations and other quantitative approaches[45] which, in most cases, are not agent-based models.[46] Further, the use of historical models to teach history has been a topic of recent interest, as models are developed into game-like applications that can be easily deployed in classroom settings.[47]
Models are particularly well suited to addressing interdisciplinary research questions. Examples include disease simulations of historical epidemics (such as the one described in this paper), models that address the transmission of knowledge and cultural behaviours within and between communities, and models that look at how mating or marriage patterns affect long-term population attributes.[48] In addition, quantitative social scientists interested in studying cultural processes have used models to address the potential outcomes of social policy or the ways that interpersonal communication plays a role in population-level behaviours.[49]
The model used here is described in some detail to illustrate how archival sources can be drawn upon to devise the structure and estimate necessary parameters for a computer simulation model. A variety of sources, including census data and parish records, photographs, and journals, have been mined for insight into the study community. Nonetheless, it is important to note that, while data from the town of St. Anthony are used to develop the model, the purpose of these data is to ensure that model structure and the values given to model parameters are as realistic as possible and can be used to test general hypotheses related to epidemic spread in similar communities, in this case small, kin-based villages. The aim of the model is not to reproduce the specific experience of St. Anthony during the pandemic.
The visualization of the St. Anthony model is a grid upon which important buildings and social spaces, represented as rectangular blocks of cells, are placed: these buildings include 84 dwellings, a school, two churches, a hospital, an orphanage, and numerous fishing boats (Figure 2). Institutions such as hospitals and orphanages were rare in most outports but were known to exist in St. Anthony because of the Grenfell Mission; thus, we have included them in our model. Because research questions focus on interactions within social spaces rather than between them (such as encounters walking along roads), the locations and proximity of buildings to each other do not reflect geographical reality. However, size and density of buildings aim to reproduce realistic conditions. For example, photographs of the orphanage indicate it was a very large building relative to the number of residents, so it is modelled as a large, loosely packed structure.
Figure 2
Visualization of the modelled community, indicating dwellings, boats, and several institutions known to exist in the study community at the time of the pandemic. Agents, represented as circles, are placed in their assigned dwellings upon initialization of the model. During the course of a simulation, agents move, often with some probability, to cells within desired destinations based on various rules of behaviour. In the current model, interactions in the hospital among medical personnel and/or patients are not considered.
When a simulation is initialized, individual agents are distributed into their assigned dwellings. Because these assignments correspond to nominal census data, the model population reflects a realistic historical community in terms of age and sex structure, family size and household distributions, and occupations. As the simulation proceeds, agents “teleport” to desired destinations, disappearing from the previous location and reappearing in the new location each time tick. Whenever a susceptible or infectious agent moves, it checks to see if it has any neighbours with the appropriate disease state to allow transmission, which happens with an assigned probability.
Like most models in epidemiology, the model used in these analyses incorporates an SEIR epidemic process that governs transmission among individuals in the model environment. The SEIR process includes four disease states — susceptible (S), exposed (or latent) (E), infectious (I), and recovered (R) — through which infected agents progress.[50] The probability of transmission and length of time spent in the exposed and infectious states are established at initialization of a simulation, as is the probability of death. For the analyses presented here, parameter estimates are derived from Newfoundland mortality data and literature on the 1918 pandemic. The lengths of the latent and infectious periods, one and three days respectively, are selected based on an assessment of different values published in the influenza literature.[51] A probability of transmission of 0.042 is used in this model to achieve a target attack rate of 55 percent prevalence during simulations, as suggested in the literature.[52] The mortality probability per tick is based on the observed death rate of about 7.5 per 1,000 people for the island of Newfoundland.[53] Given the estimated 55 percent prevalence, this rate translates to a case fatality rate of 13.6 deaths per 1,000 cases. This value is distributed uniformly across all three days (18 ticks, see below) of the infectious period; a per-tick mortality probability of 0.00076 over the 18 ticks generates a total death rate consistent with the observed data.
Behaviours and Movement
The complex behaviours and movements of agents are generally determined by age- and sex-related occupations, e.g., fishermen or schoolchildren, as well as by time period and day of the week. The model is divided into time ticks or intervals of six four-hour blocks per day. During the three daytime ticks, agent behaviours are simplified reflections of activities described in ethnographic and historical literature for residents of coastal outports in Newfoundland. For example, most male agents older than 15 years of age work in kin-based crews (relatives are assigned according to surname listed in the 1921 census) of approximately four to eight men per crew. Several males were assigned to alternate occupations, including pastors/schoolteachers and servants, based either on census data or known activities in the study community. During the fourth tick (6:00 p.m.–10:00 p.m.), agents who are outside the home at the end of the previous time tick move home; agents who are already at home at that time find a new location within the home. During the two night ticks (10:00 p.m.–2:00 a.m., 2:00 a.m.–6:00 a.m.), all agents remain immobile and “asleep” in their assigned dwellings.
Adult female agents engage in various behaviours, and the choice of these behaviours is partially based on the ages of their children, if they have any. For households with preschool-aged children (younger than five years of age), a female agent older than 15 years of age, typically the presumed mother, is assigned to be the caretaker, and the children accompany this female to any destinations during weekdays. These mothers and dependent children move within the assigned dwelling at all times except the 10:00 a.m.–2:00 p.m. interval, when they have a chance to visit other households. In households that have only school-aged or older children, all female agents older than 15 years of age also may stay home or visit, but they first decide whether to assist in the shore crew/boat during weekdays. Female caretakers responsible only for children who are ten years old or older may also participate in fishing activities on Saturdays. Regular involvement by women in shore crews is supported by multiple sources, including photographs, journals, and government and missionary reports.[54] Additionally, several adult females, as suggested by census records, are assigned to other occupations, including teachers or servants; behaviours of these agents reflect occupation status, such as movement to the school.
Behaviours of the hospital and medical staff known to be present in St. Anthony around the time of the pandemic have not yet been fully implemented in the model; therefore, agents who would otherwise be assigned to medical professions, such as doctors and nurses, have been temporarily reassigned to fishing occupations, or in one case, removed from the simulated population. Similarly, infectious agents are not yet sent to the hospital for treatment. Questions related to the impact of a medical facility in the community will be the focus of future research.
Children aged between five and 15 years old attend school during the day Monday through Friday. These schoolchildren include appropriately aged residents of the orphanage as well as community children, for orphans are assumed to attend the community school rather than receive education separately within the orphanage.[55] Ethnographic and historical evidence suggests that school attendance was likely to drop as children grew older or during busy fishing seasons. Thus, the current model assuming regular school attendance can serve as a baseline measure for future versions of the model. On Saturdays, children ten years of age and older may choose to help the shore crews/boats associated with their households. Any of these children who choose not to go to the boats, all schoolchildren younger than ten years, and children who belong to families engaged in other types of occupations may instead travel to the school to “play” with other children, visit other households with their female caretakers, or remain at home.
Finally, on Sundays, all members of a household move to a selected destination together. First, they attempt to travel to their assigned church. Churches are allowed to fill to 100 percent capacity, but the churches are not large enough to hold all community members during a single service. Thus, if there is insufficient space in the church for the full household at the time they try to go to church, the group may visit another family or remain at home. The model assumes two services each Sunday for both churches; the selection process is such that most agents have a strong but not certain chance of attending church each week. Orphans older than 15 years of age also attempt to travel to their assigned church on Sundays, but younger orphans remain in the orphanage. In between services, all agents return home.
The Disease Process
Upon initialization, all agents in the model population are classified as susceptible to influenza. Before a simulation begins, however, one agent is chosen at random as the first case, and its disease status is set to ‘exposed’. Alternatively, the first case may be chosen according to certain criteria, such as age, sex, or occupation. As described above in the discussion of SEIR models, infected agents then proceed through different disease stages. The first case, as well as any other agent who becomes infected during the remainder of the epidemic, remains in the exposed category for the length of the latent period (one day or six ticks). The infected agent then transitions to the infectious stage, which lasts three days or 18 ticks. An agent may transmit the pathogen or die from the disease only during this stage. Transmission is possible only when an infectious and susceptible pair of agents comes into contact. For the purposes of this model, sufficiently close contact is defined as agents who are in the same building or adjacent shore crews/boats, and who are neighbours to the north, south, east, or west of the reference cell. If two agents meet the necessary criteria for contact and have appropriate disease statuses, the disease still only has a chance of spreading depending on the results of a random number test. Subsequent to an infectious agent’s attempts to transmit each time tick, it also has a chance of dying, with a pre-specified mortality probability. If agents survive the infectious stage, they enter the recovered stage. In this model, recovery confers permanent immunity, so agents may not become infected again. Presently, all live agents regardless of their disease status continue to engage in regularly scheduled behaviour corresponding to their occupation status.
If an agent dies during a simulation, it may need to find a replacement for any vital occupational roles. For example, individuals who are caretakers of small children attempt to find an adult female in their household to take over childcare. If no females are available, males may become caretakers instead. Males who take over the care of older children continue to follow the same behavioural patterns as before, such as fishing or teaching. Only fishermen are allowed to care for preschool-aged children, as these new “stay-at-home-dad” caretakers give up their regular activities, at least until the dependent children die or the simulation ends. If no suitable caretakers are present in the household, all surviving children are moved to the orphanage. These childcare plans are deemed acceptable solutions due to the short time span of a single run, although alternative decisions for long-term care, such as adoption by a neighbour or relative, might be more realistic. Additionally, pastors and teachers must look for replacements for these roles among adults in the community according to age, sex, and other criteria.
Using the Model to Address Research Questions
The model described above was used to test research questions related to the role of large social institutions in the spread of disease in small communities such as those traditionally found in Newfoundland and Labrador. The first question addresses the different experiences between the orphanage and the rest of the community in St. Anthony to determine whether the observed pattern, that the wave one community epidemic did not spread to the orphanage and the wave two orphanage epidemic did not spread to the community, would be an atypical or expected outcome. The second research question explores what impact government orders and/or local community decisions to close public meeting spaces may have had on the size or timing of epidemics within the community. The results presented below focus specifically on the impact of church attendance, since that is a regular and important activity when large portions of a typical traditional community aggregate.
Test scenarios (described below) were simulated 500 times, as previous analyses indicated that this number of runs of the model sufficiently minimizes the “noise” of variation and gives results that adequately reflect average model behaviour. However, only epidemic runs, defined as five percent of the population (n = 25) ever infected, were used in further analyses. These analyses focus on measures of both epidemic size and timing. Model output allows calculation of the total number of agents ever infected, the total number of agents in the infectious stage at the peak, the time tick the peak occurred, and the last time tick at least one agent was in the infectious stage.
For the first research question, simulations of the model where an orphanage child is randomly selected to be the first case are compared to simulations where any agent in the full population may be selected as the first case. For the second research question, the model was modified so that churches would close once the epidemic reached a certain threshold, i.e., a predetermined proportion of the population became infected. Additionally, agents would no longer be allowed to visit other families on Sundays once the churches were closed, reflecting the likelihood of individual behaviour modifications in response to community-level actions. However, visiting among families during the week still took place with the same degree of probability. Church-closing thresholds of zero percent (closed at initialization), five percent, ten percent, and 100 percent (never closed) were used; the two extremes were chosen to estimate maximum positive or negative impact of such public health measures, while a threshold of five percent corresponds to the threshold for classifying a simulation as an epidemic, and ten percent was chosen under the assumption that if a public health action was not taken by the time over 50 individuals were ill within a short timeframe, it is unlikely such a decision would be made beyond that.
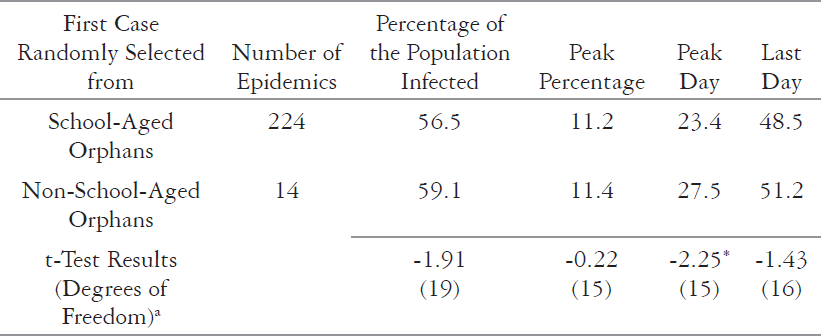
Of 500 simulations with a random orphan agent selected as the first case, nearly one-half (n=238) produced epidemics. However, the majority of those runs (n=224) were caused by school-aged orphans, indirectly indicating the importance of schools on the spread of disease throughout a community. Compared to a baseline set of epidemic simulations, where any random agent could be selected as the first case, and to the subset of these simulations excluding epidemics begun by orphans, there is no significant difference in overall percentage, percent infectious at the peak, or in the timing of the last day. Although the differences in results for the peak day are statistically significant, the absolute differences between them are small, i.e., less than two days (Table 1).
The remaining 14 epidemics in the orphan simulations typically required disease transmission from the first case to another, frequently school-aged orphan who then introduced it to the rest of the community. Simulations begun by non-school-aged orphans were thus typically delayed in both peak day and day of last infection, relative to epidemics begun by school-aged orphans. Table 2 presents results for these comparisons, which are again statistically significant only for peak day.
Simulations where churches are closed and related social behaviour is also modified during an epidemic indicate the importance of large public gathering spaces on disease spread. Although epidemics still occur readily even when movement to church and associated visiting behaviour is restricted before a simulation begins, there is a general increase in the number of people ever infected as the threshold for closure is delayed later into the course of an epidemic, except between the thresholds of five percent and ten percent (Table 3). However, this variation is minor and insignificant, whereas the changes in size for all other pairwise comparisons are statistically significant (Table 4). A similar pattern is observed for peak percentage, but no significant differences or even apparent trends are observed in the peak or final times of epidemics between any of the thresholds.
Table 1
Epidemic Outcomes Comparing Orphan and Other Selected First Cases
Table 2
Epidemic Outcomes Comparing School-Aged and Non-School-Aged Orphan First Cases
Table 3
Epidemic Outcomes Comparing Church Closure Thresholds
Table 4
Pairwise Comparisons of Final and Peak Size Outcomes for Church Closure Thresholds
Two-sample test assuming unequal variances.
The p value for this comparison is 0.052.
p < 0.05
Comparing the Model Results and the Historic Record
The St. Anthony model is designed to be a plausible representation of epidemic processes in small communities. Systematic testing of the model indicates that it produces patterns consistent with epidemiological theory and observed data from real-world epidemics. However, it is important to remember that models cannot prove what actually happened in the past, and a model that produces output consistent with observed outcomes does not necessarily capture all or indeed any of the “correct” factors that contributed to those outcomes. Nonetheless, modelling provides an opportunity to repeatedly test counterfactual scenarios, and enables researchers to estimate missing data and identify explanatory factors that may further support hypotheses generated through other research methods.
Our first research question addressed the fact that the peak time of illness in the orphanage (wave two) differed from the timing of much of the illness in the general community of St. Anthony (wave one). The recorded data suggest that the community-wide outbreak did not enter the orphanage in the first wave and the outbreak in the St. Anthony orphanage during the second wave appeared to remain effectively, if not consciously, quarantined within that institution.[56] Our comparisons of simulations that began with an orphaned child to those with the initial case chosen at random indicate few differences between the two situations. In other words, our simulations do not predict the outcome that was observed in the actual epidemic. The structure of the model, however, is such that children in the orphanage regularly attend school with other community children, thereby providing a conduit for disease spread in both the community and the orphanage that was observed in the simulations. These results suggest that one possible explanation for the historical data might be that the St. Anthony orphans of 1918 were educated separately at the orphanage or that the community school was closed prior to or during the epidemic. This emergent hypothesis prompted a return to archival sources, which revealed reports from non-pandemic years that the community school was closed at various times.[57] While these reports lack details and are for non-pandemic years, they suggest more research on education practices in the study community is necessary and present insights for modifications and additional analyses of the model. This example illustrates one important application of computer modelling for historians — to highlight possible explanations that can guide further research and provide new directions to follow when searching for archival materials.
Our analyses also demonstrate how models can be used to test counterfactual scenarios and thus explore the possible effects of various individual and community decisions on the observed outcomes. Our second research question addressed public health measures to close public spaces; the implementation of these measures likely varied in both timing and strictness in different communities. Therefore, different scenarios involving church closure and related behaviour modification were tested to determine what effect, if any, such measures may have had on disease spread. Model results suggest that these measures may have influenced the size of the epidemic in a community, sparing a portion of the population from illness. However, results also indicate that, in small, highly connected communities such as Newfoundland outports, such measures likely would not have succeeded in preventing epidemics entirely or even slowing them down, if other regular activities and interactions continued. The relatively large difference in outcomes when the church is closed prior to the beginning of the simulation and when it is closed after a mere five percent of the population has been infected, as well as the lack of statistical significance in the difference between outcomes at thresholds of five and ten percent, suggest that action must be taken early, indeed even prior to the epidemic reaching a particular community, to have an effect. These results reinforce observations from the historic record that community-level experiences varied widely and that less severe outbreaks probably resulted from a variety of factors beyond simply prohibiting aggregation of community members.
The analyses for these two research questions demonstrate the usefulness of models for generating possible explanations of observed historical phenomena. In a sense, historical data, such as the recorded number of cases and deaths during an epidemic, the subsequent community and individual responses, and the effect of those responses, can be considered comparable to one “simulation” out of a wide range of possible outcomes. Models that are well-constructed and informed by validated data sources are able to determine what this range of possibility is, what outcomes are more or less typical or plausible, and what factors might have been particularly important in producing those outcomes. The analyses presented here highlight two applications of modelling research to historical studies — accommodating gaps in the archival record and exploring counterfactual scenarios. Further, major advances in computing hardware and the availability of affordable, user-friendly software make computer modelling an attractive option for researchers.
A major constraint for developing agent-based models is the availability and quality of necessary data for the population and phenomenon under study. Model developers encounter similar difficulties as traditional historians do, including limited or restricted access to archival data, damaged or lost records, and the need to evaluate sources for authenticity and validity. Particularly in the case of historical health events, individuals most commonly engaged in modelling activities, such as biologists, mathematicians, and anthropologists, frequently do not have sufficient training in finding and evaluating archival and historical sources. However, members of these fields are often highly trained in biological and/or social and behavioural science methodologies and concerns. Therefore, collaboration between historians and researchers in other disciplines presents opportunities for a broader understanding and investigation of historical epidemics or other events through integration of modelling techniques with more traditional research strategies.
Appendices
Acknowledgements
The authors would like to acknowledge the support of the Government of Canada-Canada Studies Faculty Research Grant Program, the University of Missouri Columbia Research Council, and the University of Missouri Research Board. Additionally, we thank Erin Miller and Amy Warren for contributions to model development and insights into this project.
Biographical notes
JESSICA DIMKA is a Ph.D. candidate in Anthropology at the University of Missouri Columbia. Her research interests include the role of social networks and individual behaviours on the spread of infectious diseases within communities, as well as the consequent health outcomes for different sex and age groups.
CAROLYN ORBANN is an Assistant Teaching Professor of Health Sciences at the University of Missouri Columbia. Her research interests include the role of large scale population contact on the spread of infectious disease, particularly during the colonial period in North America.
LISA SATTENSPIEL is a Professor of Anthropology at the University of Missouri Columbia. Her research specialty is the study of how social activities and population movements influence the spread of infectious diseases in both past and present populations.
Notes
-
[1]
See, for example, Frederick F. Cartwright, Disease and History (New York: Thomas Y Crowell, 1972); Alfred W. Crosby, Epidemics and Peace, 1918 (Westport, CT: Greenwood, 1976), reprinted under the title America’s Forgotten Pandemic: The Influenza of 1918 (Cambridge: Cambridge University Press, 1989); René Dubos and Jean Dubos, The White Plague: Tuberculosis, Man, and Society (Boston: Little, Brown & Company, 1952); William H. McNeill, Plagues and Peoples (Garden City, NY: Anchor Press, 1976); Terence Ranger and Paul Slack, eds. Epidemics and Ideas: Essays on the Historical Perception of Pestilence (Cambridge: Cambridge University Press, 1992); Charles E. Rosenberg, The Cholera Years: The United States in 1832, 1849 and 1866 (Chicago: University of Chicago Press, 1962); and Sheldon Watts, Epidemics and History: Disease, Power and Imperialism (New Haven, CT: Yale University Press, 1999).
-
[2]
John Bonnett, “Historians and Technology/Les historiens et la technologie,” Canadian Historical Association Featured Articles, http://www.cha-shc.ca/download.php?id=1495, <viewed 24 August 2014>.
-
[3]
Magna Fahrni and Esyllt Jones, “Introduction” in Epidemic Encounters: Influenza, Society, and Culture in Canada, 1918–1920, eds. Magda Fahrni and Esyllt W. Jones (Vancouver: University of British Columbia Press, 2012), 1–18; Niall P. A. S. Johnson and Juergen Mueller, “Updating the Accounts: Global Mortality of the 1918–1920 “Spanish” Influenza Pandemic,” Bulletin of the History of Medicine 76, no.1 (2002): 105–15.
-
[4]
Johnson and Mueller, “Updating the Accounts,” 114.
-
[5]
Svenn-Erik Mamelund, Lisa Sattenspiel, and Jessica Dimka, “Influenza-Associated Mortality During the 1918–1919 Influenza Pandemic in Alaska and Labrador: A Comparison,” Social Science History 37, no. 2 (2013): 177–229.
-
[6]
Early analyses of the number and timing of waves were first presented by Warren Taylor Vaughan, “Influenza: An Epidemiologic Study,” American Journal of Hygiene Monograph Series No. 1 (1921). Subsequent discussion and expansion of these findings have been contributed by researchers including Crosby, Epidemics and Peace, 1918; J. S. Oxford, “The So-Called Great Spanish Influenza Pandemic of 1918 May Have Originated in France in 1916,” Philosophical Transactions of the Royal Society of London, Series B – Biological Sciences 356 (2001): 1857–9; J. S. Oxford, A. Sefton, R. Jackson, W. Innes, R. S. Daniels, and N. P. A. S. Johnson, “World War I May Have Allowed the Emergence of ‘Spanish’ Influenza,” The Lancet Infectious Diseases 2, no. 2 (2002): 111–4.
-
[7]
Crosby, Epidemics and Peace, 1918; Oxford et al., “World War I May Have Allowed.”
-
[8]
Mark Osborne Humphries, “The Horror at Home: The Canadian Military and the “Great” Influenza Pandemic of 1918,” Journal of the Canadian Historical Association 16, no. 1 (2005): 235–60.
-
[9]
See, for example, G. Chowell, C. E. Ammon, N. W. Hengartner, and J. M. Hyman, “Transmission Dynamics of the Great Influenza Pandemic of 1918 in Geneva, Switzerland: Assessing the Effects of Hypothetical Interventions,” Journal of Theoretical Biology 241, no. 2 (2006): 193–204; Crosby, Epidemics and Peace, 1918; Edwin O. Jordan, Epidemic Influenza: A Survey (Chicago: American Medical Association, 1927); Howard Markel, Harvey B. Lipman, J. Alexander Navarro, Alexandra Sloan, Joseph R. Michalsen, Alexandra Minna Stern, and Martin S. Cetron, “Nonpharmaceutical Interventions Implemented by US Cities During the 1918–1919 Influenza Pandemic,” Journal of the American Medical Association 298, no. 6 (2007): 644–54.
-
[10]
Donald R. Olson, Lone Simonsen, Paul J. Edelson, and Stephen S. Morse, “Epidemiological Evidence of an Early Wave of the 1918 Influenza Pandemic in New York City,” Proceedings of the National Academy of Sciences of the United States of America 102, no. 31 (2005): 11059–63.
-
[11]
See, for example, Gerardo Chowell, Luís M. A. Bettencourt, Niall Johnson, Wladimir J. Alonso, and Cécile Viboud, “The 1918–1919 Influenza Pandemic in England and Wales: Spatial Patterns in Transmissibility and Mortality Impact,” Proceedings of the Royal Society B 275, no. 1634 (2008): 501–9; Andrew Noymer and Michel Garenne, “The 1918 Influenza Epidemic’s Effects on Sex Differentials in Mortality in the United States,” Population and Development Review 26, no. 3 (2000): 565–81; Lisa Sattenspiel and Svenn-Erik Mamelund, “Co-Circulating Epidemics, Chronic Health Problems, and Social Conditions in Early 20th Century Labrador and Alaska,” Annals of Anthropological Practice 36, no. 2 (2013): 402–21.
-
[12]
Howard Phillips, “The Recent Wave of ‘Spanish’ Flu Historiography,” Social History of Medicine 27, no. 4 (2014): 789–808. Note that the term “second wave” indicates a shift in research questions from earlier studies into the pandemic and also is used as a pun to reflect frequent focus on the second wave of the pandemic. As Phillips writes on page 790, “Like the second wave of that pandemic, the historiography of ‘Spanish’ flu has also exploded.”
-
[13]
Jane E. Jenkins, “Baptism of Fire: New Brunswick’s Public Health Movement and the 1918 Influenza Epidemic,” Canadian Bulletin of Medical History 24, no. 2 (2007): 317–42; Heather MacDougall, “Toronto’s Health Department in Action: Influenza in 1918 and SARS in 2003,” Journal of the History of Medicine and Allied Sciences 62, no. 1 (2006): 56–89.
-
[14]
Esyllt W. Jones, “Contact Across a Diseased Boundary: Urban Space and Social Interaction During Winnipeg’s Influenza Epidemic, 1918–1919,” Journal of the Canadian Historical Association 13, no. 1 (2002): 119–39; Linda J. Quiney, “’Filling the Gaps’: Canadian Voluntary Nurses, the 1917 Halifax Explosion, and the Influenza Epidemic of 1918,” Canadian Bulletin of Medical History 19, no. 2 (2002): 351–74.
-
[15]
Jones, “Contact Across a Diseased Boundary”; Esyllt Jones, “Politicizing the Laboring Body: Working Families, Death, and Burial in Winnipeg’s Influenza Epidemic, 1918–1919,” Labor: Studies in Working-Class History of the Americas 3, no. 3 (2006): 57–75; see also Esyllt W. Jones, Influenza 1918: Disease, Death, and Struggle in Winnipeg (Toronto: University of Toronto Press, 2007) for a comprehensive discussion of the Winnipeg experience; Mary-Ellen Kelm, “British Columbia First Nations and the Influenza Pandemic of 1918–19,” BC Studies 122 (1999): 23–48.
-
[16]
Magda Fahrni and Esyllt W. Jones, eds., Epidemic Encounters: Influenza, Society, and Culture in Canada, 1918–1920 (Vancouver: University of British Columbia Press, 2012).
-
[17]
Fahrni and Jones, “Introduction,” 16.
-
[18]
Mamelund et al., “Influenza-Associated Mortality,” 178; Lisa Sattenspiel, “Regional Patterns of Mortality during the 1918 Influenza Pandemic in Newfoundland,” Vaccine 29S (2011): B33–7.
-
[19]
Sattenspiel, “Regional Patterns,” B35.
-
[20]
Ibid., B35–6.
-
[21]
Bowring Brothers, Limited, “Sealing Crews!” Evening Telegram (St. John’s, NL), 28 February 1919; Job Brothers & Company, Limited, “Notice to Sealers!” Evening Telegram (St. John’s, NL) 28 February 1919.
-
[22]
Mamelund et al., “Influenza-Associated Mortality,” 215.
-
[23]
Notices and articles regarding closures of public gathering places appeared in both the Evening Telegram and Daily News, both published in St. John’s, NL, during the epidemic. Correspondence found in the Provincial Archives of Newfoundland and Labrador (PANL), GN 2/5, Special File no. 352-A; Correspondence Regarding Outbreak of Spanish Influenza in Newfoundland, letter dated 2 November 1918, indicates that these restrictions were applicable only to St. John’s.
-
[24]
The Literature Committee of the Diocesan Synod of Newfoundland, St. John’s, “What our Diocese is Doing,” The Diocesan Magazine, Newfoundland 31, no. 3 (1919): 49.
-
[25]
Carolyn Orbann, Jessica Dimka, Erin Miller, and Lisa Sattenspiel, “Agent-Based Modeling and the Second Epidemiologic Transition” in Modern Environments and Human Health: Revisiting the Second Epidemiologic Transition, ed. Molly K. Zuckerman (Hoboken, NJ: Wiley-Blackwell, 2014), 105–22; Sattenspiel, “Regional Patterns,” B33.
-
[26]
See, for example, Melvin M. Firestone, Brothers and Rivals: Patrilocality in Savage Cove, Newfoundland Social and Economic Studies, ARDA Project No. 1016, No. 5 (St. John’s, Newfoundland: Memorial University of Newfoundland, 1967); Thomas F. Nemec, “I Fish with My Brother: The Structure and Behaviour of Agnatic-Based Fishing Crews in a Newfoundland Irish Outport” in North Atlantic Fishermen: Anthropological Essays on Modern Fishing, eds. Raoul Andersen and Cato Wadel, Newfoundland Social and Economic Papers No. 5 (St. John’s, NL: Institute of Social and Economic Research, Memorial University of Newfoundland, 1972), 9–34; Stuart A. Queen and Robert W. Habenstein, The Family in Various Cultures, 4th ed. (Philadelphia: JB Lippincott, 1974).
-
[27]
Queen and Habenstein, The Family in Various Cultures.
-
[28]
Hilda Chaulk Murray, More than Fifty Percent: Woman’s Life in a Newfoundland Outport 1900–1950, Canada’s Atlantic Folklore and Folklife Series No. 3 (St. John’s, NL: Breakwater Books, 1979); Marilyn Porter, “‘She Was Skipper of the Shore-Crew:’ Notes on the History of the Sexual Division of Labour in Newfoundland,” Labour/LeTravail 15 (1985): 105–23.
-
[29]
John Feltham, The Islands of Bonavista Bay (St. John’s, Newfoundland: Harry Cuff Publications Limited, 1986); Gerald L. Pocius, “Hooked Rugs in Newfoundland: The Representation of Social Structure in Design,” The Journal of American Folklore 92, no. 365 (1979): 273–84.
-
[30]
Marilyn Beaton and Jeanette Walsh, From the Voices of Nurses: An Oral History of Newfoundland Nurses who Graduated Prior to 1950 (St. John’s, NL: Jesperson Publishing, 2004); Sean T. Cadigan, Newfoundland and Labrador: A History (Toronto: University of Toronto Press, 2009); Janet E. Miller Pitt and Melvin Baker, “Health” in Encyclopedia of Newfoundland and Labrador, ed. J.R. Smallwood (St. John’s, NL: Newfoundland Book Publishers, 1984), 2: 864–75.
-
[31]
Cadigan, Newfoundland and Labrador: A History, 206.
-
[32]
Beaton and Walsh, From the Voices of Nurses, 126.
-
[33]
R. A. Vandelehr and Roger E. Heering, Report of a Survey on Civil Health Services as They Relate to the Health of Armed Forces in Newfoundland (United States Public Health Service, 1940), reprinted in James E. Candow, “An American Report on Newfoundland’s Health Services in 1940,” Newfoundland and Labrador Studies 5, no. 2 (1989): 221–39. The quote appears in Candow’s commentary on p. 222 and in the report itself on p. 226 of Candow.
-
[34]
Pitt and Baker, “Health”; Vandelehr and Heering (Candow), “An American Report,” 230.
-
[35]
S. B. Sniffen and M. Schreiber, “New York to Spotted Islands,” Among the Deep Sea Fishers 20, no. 1 (1922): 10–4; Gordon W. Thomas, From Sled to Satellite: My Years with the Grenfell Mission (Self-copyright, 1987), 24.
-
[36]
Patricia A. Green, “Health (Nutrition)” in Encyclopedia of Newfoundland and Labrador, ed. J. R. Smallwood (St. John’s, NL: Newfoundland Book Publishers, 1984), 2: 880–9.
-
[37]
Newfoundland Colonial Secretary’s Office, Census of Newfoundland and Labrador, 1921 (St. John’s, NL: Colonial Secretary’s Office, 1923).
-
[38]
John C. Kennedy, People of the Bays and Headlands: Anthropological History and the Fate of Communities in Unknown Labrador (Toronto: University of Toronto Press, 1995).
-
[39]
Among the Deep Sea Fishers documented the activities of the Grenfell Mission in an engaging way that encouraged readers to support those activities financially. As such it is filled with detailed articles about all aspects of life in the Northern Peninsula of Newfoundland and in Labrador throughout the time period of its publication.
-
[40]
Charles S. Curtis Memorial Hospital, St. Anthony, NL, unpublished records.
-
[41]
K. Spalding, “Report of the Orphanage,” Among the Deep Sea Fishers 17, no. 4 (1920): 139–40.
-
[42]
Craig T. Palmer, Lisa Sattenspiel, and Chris Cassidy, “Boats, Trains, and Immunity: The Spread of the Spanish Flu on the Island of Newfoundland,” Newfoundland and Labrador Studies 22, no 2 (2007): 473–504.
-
[43]
International Grenfell Association Archives, St. Anthony, NL, unpublished orphanage health records.
-
[44]
See, for example, the special issue of Simulation and Gaming, 42, no. 4 (2011).
-
[45]
Michael J. Armstrong and Michael B. Powell, “A Stochastic Salvo Model Analysis of the Battle of the Coral Sea,” Military Operations Research 10, no. 4 (2005): 27–37.
-
[46]
Thomas W. Lucas, “The Stochastic Versus Deterministic Argument for Combat Simulations: Tales of When the Average Won’t Do,” Military Operations Research 5, no. 3 (2000): 9–28.
-
[47]
Pierre Corbeil, “History and the Computer in Canadian Institutions: An Overview,” Social Science Computer Review 23, no. 2 (2005): 181–9; Bruce E. Rigelow, “Simulation Review: Simulations in History,” Simulation and Gaming 9, no. 2 (1978): 209–20.
-
[48]
Francesco C. Billari, Alexia Prskawetz, Belinda Aparicio Diaz, and Thomas Fent, “The ‘Wedding-Ring’: An Agent-Based Marriage Model Based on Social Interaction,” Demographic Research 17 (2008): 59; Joshua M. Epstein, Generative Social Science: Studies in Agent-Based Computational Modeling (Princeton, N.J.: Princeton University Press, 2006); John P. Gilbert and E. A. Hammel, “Computer Simulation and Analysis of Problems in Kinship and Social Structure,” American Anthropologist 68, no. 1 (1966): 71–93; Petter Holme and Andreas Grönlund, “Modelling the Dynamics of Youth Subcultures,” Journal of Artificial Societies and Social Simulation 8, no. 3 (2005): 3 <http://jasss.soc.surrey.ac.uk/8/3/3.html>; Alex Mesoudi and Michael J. O’Brien, “The Cultural Transmission of Great Basin Projectile-Point Technology II: An Agent-Based Computer Simulation,” American Antiquity 73, no. 4 (2008): 627–44.
-
[49]
Robert Axelrod, “The Dissemination of Culture: A Model with Local Convergence and Global Polarization,” Journal of Conflict Resolution 41, no. 2 (1997): 203-26; Thomas Berger, “Agent-Based Spatial Models Applied to Agriculture: A Simulation Tool for Technology Diffusion, Resource Use Changes and Policy Analysis,” Agricultural Economics 25, no. 2-3 (2001): 245–60; Michael W. Macy and Robert Willer, “From Factors to Actors: Computational Sociology and Agent-Based Modeling,” Annual Review of Sociology 28 (2002): 143–66.
-
[50]
See, for example, Roy M. Anderson and Robert McCredie May, Infectious Diseases of Humans: Dynamics and Control (Oxford: Oxford University Press, 1991); Herbert W. Hethcote, “The Mathematics of Infectious Diseases,” SIAM Review 42, no. 4 (2000): 599–653; and Matt J. Keeling and Pejman Rohani, Modeling Infectious Diseases in Humans and Animals (Princeton, N.J.: Princeton University Press, 2008).
-
[51]
See, for example, A. Cori, A. J. Valleron, F. Carrat, G. Scalia Tomba, G. Thomas, and P. Y. Boëlle, “Estimating Influenza Latency and Infectious Period Durations Using Viral Excretion Data,” Epidemics 4, no. 3 (2012): 132–8; Christina E. Mills, James M. Robins and Marc Lipsitch, “Transmissibility of 1918 Pandemic Influenza,” Nature 432, no. 7019 (2004): 904–6.
-
[52]
Neil M. Ferguson, Derek A. T. Cummings, Simon Cauchemez, Christophe Fraser, Steven Riley, Aronrag Meeyai, Sopon Iamsirithaworn, and Donald S. Burke, “Strategies for Containing an Emerging Influenza Pandemic in Southeast Asia,” Nature 437, no. 7056 (2005): 209–14.
-
[53]
Sattenspiel, “Regional Patterns,” B35.
-
[54]
For example, Murray, More than Fifty Percent; Porter, “She Was Skipper of the Shore-Crew”; Queen and Habenstein, The Family in Various Cultures.
-
[55]
A recently unearthed source (Frances Baier, “The New Orphanage,” Among the Deep Sea Fishers 22, no. 2 (1924): 54–7) indicates that orphanage residents attended the community school in the mornings only. This information has not yet been implemented into the model; it assumes at present that all schoolchildren attend all day. Future versions of the model will incorporate this new evidence, which may offer further insight into the different epidemic experiences between the orphanage and the community as a whole.
-
[56]
No evidence of a quarantine order has yet been found in records held by the International Grenfell Association in St. Anthony. However, reports published in Among the Deep Sea Fishers indicate that, while the community school apparently did not receive financial support from the government, the orphanage received approximately 18–25 percent of its budget each year from government support. Further, reports often included descriptions of health-related issues in the orphanage, such as disease outbreaks, and infrastructure development, such as improvements to the water supply. Inclusion of this kind of information suggests that, if a quarantine had been ordered and/or implemented, it would be addressed in the reports.
-
[57]
A 1914 report in Among the Deep Sea Fishers, for example, indicates that the community school was closed during the winter and orphans were taught by volunteer teachers, further suggesting the orphanage children attended the school when it was open.
Appendices
Notes biographiques
JESSICA DIMKA est doctorante en anthropologie à l’Université du Missouri à Columbia. Sa recherche porte sur le rôle des réseaux sociaux et du comportement individuel dans la propagation de maladies infectieuses au sein de collectivités ainsi que sur les effets afférents pour la santé en fonction du sexe et de l’âge.
CAROLYN ORBANN est professeure adjointe au département des sciences de la santé de l’Université du Missouri à Columbia. Sa recherche porte sur le rôle des contacts de population à grande échelle dans la propagation de maladies infectieuses, notamment durant la période coloniale en Amérique du Nord.
LISA SATTENSPIEL est professeure d’anthropologie à l’Université du Missouri à Columbia. Sa recherche cible les façons dont les activités sociales et les mouvements de population influencent la propagation de maladies infectieuses tant aujourd’hui que dans le passé.
List of figures
Figure 1
Figure 2
Visualization of the modelled community, indicating dwellings, boats, and several institutions known to exist in the study community at the time of the pandemic. Agents, represented as circles, are placed in their assigned dwellings upon initialization of the model. During the course of a simulation, agents move, often with some probability, to cells within desired destinations based on various rules of behaviour. In the current model, interactions in the hospital among medical personnel and/or patients are not considered.
List of tables
Table 1
Epidemic Outcomes Comparing Orphan and Other Selected First Cases
Table 2
Epidemic Outcomes Comparing School-Aged and Non-School-Aged Orphan First Cases
Table 3
Epidemic Outcomes Comparing Church Closure Thresholds
Table 4
Pairwise Comparisons of Final and Peak Size Outcomes for Church Closure Thresholds