Résumés
Abstract
In the mid 1940s the Canadian government implemented a medical mass-survey of Inuit and other Indigenous peoples living in northern Canada, and evacuated those suspected of having tuberculosis to hospitals in the south. Hospital stays often lasted for years at a time and while some patients were eventually returned to their home communities, many never returned, some because they chose to stay in the south and others because they did not survive their illness. The current study is interested in how hospitalisation in the south affected the identity of Inuit patients, and in particular examines the negotiation of identity as a form of resilience. This investigation is conducted through life history interviews with Inuit former evacuees in which we explore their experiences of departure, travel, and sojourn in an unfamiliar environment, as well as their lives after the hospital stay.
Résumé
Au milieu des années 1940, le gouvernement canadien réalisa un examen de dépistage auprès des Inuit et autres populations autochtones qui habitaient au nord du Canada et évacua ceux qui présentaient des symptômes de la tuberculose vers les hôpitaux du sud. Les séjours à l’hôpital durèrent souvent des années et alors que certains patients furent retournés plus tard à leurs communautés respectives, plusieurs ne regagnèrent jamais celles-ci parce qu’ils décidèrent de rester dans le sud et d’autres, parce qu’ils ne survécurent pas à leur maladie. La présente étude analyse comment l’hospitalisation dans le sud affecta l’identité des patients inuit et examine notamment la négociation de l’identité comme forme de résilience. Cette recherche a été menée par le biais d’entrevues auprès d’anciens évacués inuit sur leur expérience de vie et aborde les événements entourant les départs, les déplacements, les séjours dans un nouvel environnement et la vie après un séjour à l’hôpital.
Corps de l’article
In memory of Johanna Rabinowitz
We left [home] without knowing any Qallunaaq[1] ways whatsoever. It was like as if they turned us into White as soon as we entered into that building.
Pauloosie Kanayuk, 2005
Introduction
In 1946, the Canadian government implemented a medical mass-survey of Inuit and other Aboriginal peoples living in northern Canada and began the evacuation of those suspected of having tuberculosis (TB) and other serious conditions. The tuberculosis epidemic among the Inuit population of Canada took a heavy toll on many families, camps and settlements (Grygier 1994: 54; Grzybowski et al. 1976: 1-3). The literature suggests that at the height of the evacuation in the mid-1950s approximately 7 to 10% of the Inuit population of Canada was hospitalised with tuberculosis (Duffy 1988: 71; Grygier 1994: 71; Jenness 1972: 143,146). Hospital stays often lasted several years, and while many Inuit were returned to their home communities, others never returned, some because they chose to stay in the south, some because their resulting disabilities were too severe to allow for them to return to their life on the land, and others because they did not survive their illness (Grygier 1994: xxi, 143-151). Nearly every Inuit community today includes among its numbers individuals, often children at the time, who were evacuated and returned years later from TB treatment in the south. As a result, the TB epidemic and subsequent evacuation had great impact not only on individual lives but also on Inuit community and culture.
The current article is part of a research project involving life history interviews with former Inuit TB patients and former medical personnel. It explores the impact of the evacuation and the negotiation of identity embedded within the discourses of former TB evacuees. The hospital stay, struggling with illness, and the return to the community were difficult periods in the lives of these former patients, children and young adults who were removed from their homes and families in the North and transplanted across cultures and country. In this article, through the words of our participants, we will describe how they negotiate their changing environment and fluctuating identities from past to present, through suffering and illness, coping and survival, leaving for the South and returning to the North. The present study focuses on Inuit participants who originated from northern Quebec, known today as Nunavik. Some of them remain in Nunavik to this day, while others have settled in Montreal and Ottawa. We will begin by briefly outlining the history of tuberculosis among the Inuit of Canada before moving on to explore the narratives of the participants. This paper will conclude with a discussion of the negotiation of identity as a form of resilience (Holton et al. in press).
Tuberculosis among the Inuit of Canada
Tuberculosis is a potentially deadly contagious bacterial infection that is typically seen in the lungs, although it may attack other parts of the body as well (Long 2000). The disease was feared across Europe and North America until the 1940s and 1950s when the development and use of antibiotic drugs efficient against mycobacterium tuberculosis allowed for a potential cure (Grygier 1994: 11).
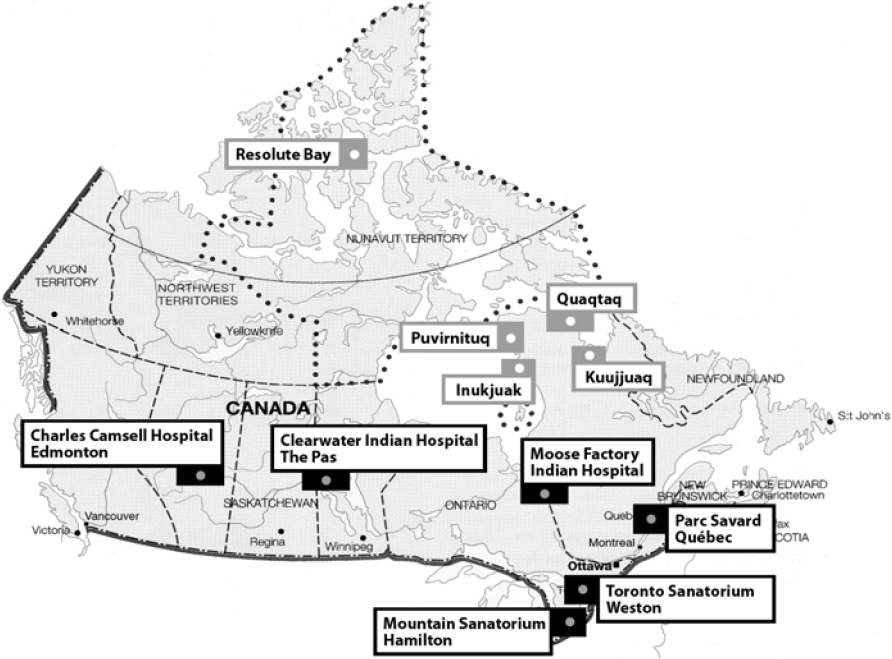
Although the Canadian federal government was officially responsible for the health care and medical services of the Inuit, little was provided prior to 1940. Despite the fact that great numbers of the Inuit population were suffering from TB, only a few severe cases were evacuated to hospitals in the south (Grygier 1994: 55-65; Vanast 1991). The Inuit and those stationed up North had to fend for themselves, with the Royal Canadian Mounted Police (RCMP), the missionaries and the Hudson Bay Company traders often acting as health care providers (Grygier 1994: 41-51; Imaapik “Jacob” Partridge, 2007; Vanast 1991). It was not until 1946, when the “Advisory Committee for the Control and Prevention of Tuberculosis among Indians” was formally set up, that something was done to help the Inuit and the other Aboriginal peoples living in the North (Grygier 1994: 63; Wherrett 1977: 116-117). While there already existed a few hospitals in the Northwest Territories and in northern Quebec, these hospitals did not have the capacity to treat tuberculosis patients if they needed specialised care. The federal government made the decision not to build any new hospitals in the North, nor to enlarge the existing ones, and instead chose to implement a large scale evacuation of Inuit who were ill with TB to hospitals and sanatoriums in southern Canada (Grygier 1994: 55-65, 73, 195; Jenness 1972: 84-86) (Figure 1).
Prior to the launch of the medical evacuation, a ship would travel almost yearly from Montreal to Churchill along the coast of Labrador to different Inuit communities in northern Quebec, as well as the Eastern and High Arctic, before returning to Montreal. This was known as the “Eastern Arctic Patrol,” used mainly for supplying goods to the Hudson Bay Company trading posts and for conducting a variety of surveys. The ship was usually attended by a medical officer (Grygier 1994: 43-44; Phillips 1957). In 1946, when the governmental medical evacuation program was implemented, the Eastern Arctic Patrol was equipped with medical personnel, including a medical officer, nurses, nurse aides, and a dentist, X-ray equipment, and X-ray technicians. The first ship used for the medical evacuation program was the Nascopie, later replaced by the C.D. Howe, which was equipped with a helicopter, allowing patients to be evacuated by air if necessary. Known as the “hospital boat,” the C.D. Howe was used in the Eastern Arctic Patrol, and consequently for the medical evacuation program, until the Patrol was discontinued in 1969 (Grygier 1994: 86).
The Inuit were examined according to a strict routine on board the hospital ship of the Eastern Arctic Patrol (Figure 2). An interpreter (if available on board) would be the first to register the potential patient with name and disk number[2]. A serial number was written on the arm or on the right hand following the order in which they were seen on the boat by the medical personnel. The potential patients would then have their chest X-ray taken, be examined by a physician and a dentist, and immunised by a nurse. The X-rays were developed on the boat. Letters were printed on the left hand as the individual went through the examinations: X P D I, representing the X-ray, Physician, Dentist, and Immunisation. If the person was found to be free of tuberculosis or other serious illness, an arrow was printed under the letters, indicating he or she could go home (Figure 3). If found to be ill with tuberculosis then the letters TB were printed on the patient’s hand and he or she would be transported to the South as soon as the boat was ready for departure, sometimes merely hours after the patient was examined (Figure 4) (Grygier 1994: 66-71; Johanna Rabinowitz, 2005, 2006, 2007; Willis 1956).
Figure 1
Map showing the hospitals and sanatoriums used for TB in Canada.
Going to the hospital…
There were a lot of us who were forced to get married the day before we left to go to the hospital and the minister performed the wedding ceremony for us and some people went to die.
Mary Johnson[3], 2005
Being told that they had to leave with the hospital boat or airplane to go to a hospital in the South was a frightening experience for most of the patients. They had seen other members of the community, friends and relatives leave for a hospital in the South, never to return. While some of the Inuit ill with TB were aware that they had a serious illness, many were diagnosed while still asymptomatic, and as such there was often great confusion as to why they were being taken from their homes and families. Even when they were aware of their condition, it was not always made clear to the patients where they were being taken or if they would ever be returned, contributing to an atmosphere of fear and desperation. In some cases, Inuit who knew that they were seriously ill would hide out on the land once they had heard that the hospital boat was arriving. In these situations, a helicopter, originally intended to fly ahead of the boat to check ice conditions or bring medical personnel to shore if the boat could not dock, was used to survey the land, find anyone hiding, and bring them to the boat for examination (Johanna Rabinowitz 2005, 2006, 2007).
Family members were not allowed to accompany the ill. Children, even infants, who were diagnosed with TB would be taken from their parents and sent with the boat. Men and women would be forced to leave their families behind, without any knowledge of their destination or if they would return. Families suffered not only emotional distress, but were faced with challenges to their survival, at times left without a father to hunt or a mother to make clothes or care for the children. Evacuees in turn faced great emotional distress, knowing that it would be difficult for their family to survive without them. As exemplified in the quote above, so great was the desperation, that the minister would often marry couples when one of them had to leave for the hospital, in order to sanctify the union while there was still time to do so.
Figure 2
People waiting in line for medical examination on board the C.D. Howe.
Figure 3
Markings on the hands.
Figure 4
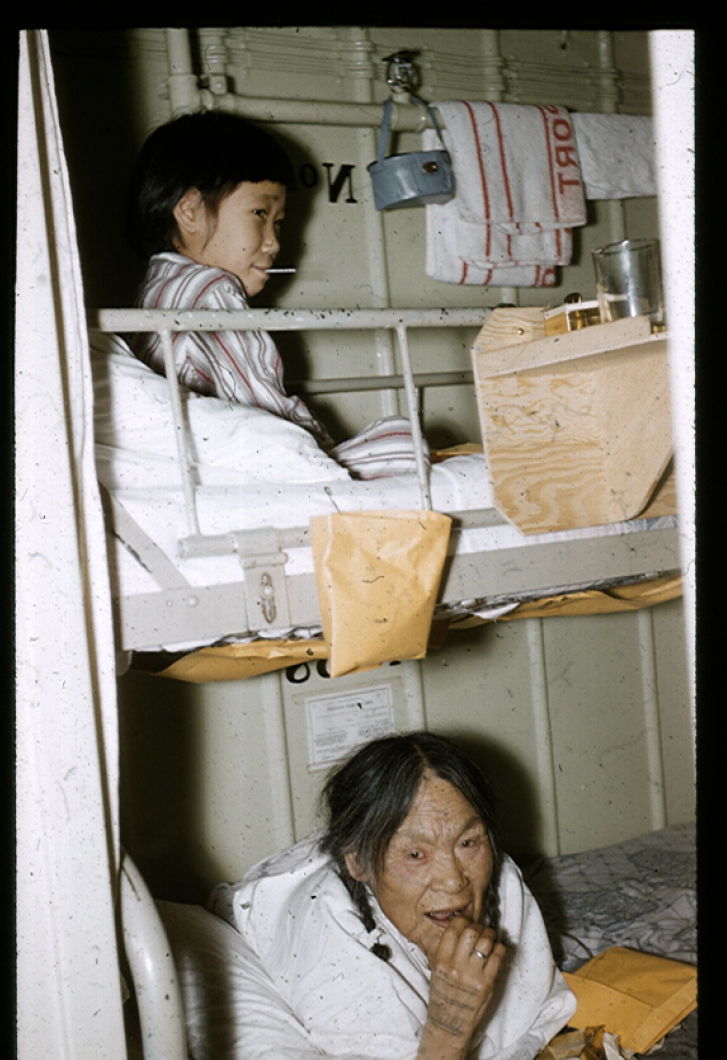
A child and an elder woman in bed on board the C.D. Howe.
Although the Inuit ill with TB were reluctant to leave and fearful of what might happen to them and their families, most went without question, some because they recognised that they were ill and felt that the hospitals in the South were their only hope, while others left in part because they did not feel it was within their power to refuse. Many felt intimidated by non-Inuit Canadians, the police, the minister, and others working in the North. This feeling of fearing someone because he or she is intimidating, known in Inuktitut as ilira, is described both by Brody (2000: 216-220) and Marcus (1994: 79). A lack of proper record keeping and registration of patients added to the confusion and hardship faced by Inuit communities. Although the “Eskimo Disk List System” was already in use by the early 1940s (Smith 1993: 60-63), patients were sometimes registered with the wrong name and disk number, and names were sometimes written down incorrectly even if the patient had a Christian (English) name (Grygier 1994: 115-128).
The nurse that registered me could not find my name on the list. My Christian name is in reality Matthew, today the name of my son. She put me down as Jacob, a name that she found on the list, so I also got his disk number which created a lot of problems when I was discharged from the hospital and was supposed to be sent home. At least she put down the last name of my mother so she got my last name right. Although my mother argued with the nurse that my name was Matthew not Jacob, the nurse would not give in and so I was sent to the hospital as Jacob. And that has been my name since then.
Imaapik “Jacob” Partridge, 2007
Relatives of the patients often were unaware of where their family members had been taken, and patients were sometimes sent home to the wrong community. There were problems in communication between the hospitals and Inuit communities so the information that a patient had died while in the hospital did not always reach their relatives (Grygier 1994: 115-128).
It must be noted that it would be a misrepresentation to portray the Inuit as simply forced against their will to seek medical treatment. Some chose to endure the fear and confusion resulting from being seen by the medical personnel in the hopes of finding help for themselves or their family members. For Markoosie Patsauq his illness was so pronounced that both he and his family recognised he would have to be evacuated to the hospital.
In my family, especially my mother used to say, “probably you’re going to the hospital.” I was kind of scared. I had never been away from the family before. So when the news comes around that I have a bad TB, I wasn’t surprised and my family knew I had it a year ago.
Markoosie Patsauq, 2005
Some families went to great lengths to find help for their children. Imaapik “Jacob” Partridge was an infant when he developed tuberculosis in his hip bone, which prevented him from learning to walk. At this time, in the early 1940s there was limited access to medical care in the Quaqtaq area where he and his family lived. In an attempt to help Imaapik and his family, an RCMP officer gave him two injections in his hip from which he got an infection. The RCMP officer informed Imaapik’s parents that they could seek medical care for him in Kuujjuaq, and so they did; when the ice melted, the whole family travelled by boat to Kuujjuaq. There it was decided that he would be flown out to Goose Bay, and later on, he was transferred to the Weston Hospital Complex in Toronto, to the Queen Mary Hospital for children with TB (Imaapik “Jacob” Partridge, 2007).
The hospital stay
What we went through helped us to get well again, but it certainly had an impact on our lives. If only all of the people working at the hospital were more understanding and especially if only some of the interpreters were more helpful with the patients it could have minimised negative impact on some of the patients […].We didn't know who was responsible for running the situation we were in, we didn’t know whether it was the government or who were the people responsible of the whole thing.
Pauloosie Kanayuk, 2005
After what was often a difficult journey either by boat or plane, followed by a train or bus ride, the patients would arrive at the hospital. Inuit patients were often seriously ill with advanced tuberculosis and had never before travelled by plane, train or bus. Most were overwhelmed by their surroundings, having never travelled so far from home and to an environment that was starkly different from that of their home community. For some it was the first time they had seen a tree or building, the first time they were to take a shower or use a flush toilet, and they had no idea where they were (Grygier 1994: 104-116). Patients did not speak English or French and there was seldom a competent interpreter at the hospital to help them orient themselves. If an interpreter was present, it was often a patient or a former patient. Some felt poorly treated by the interpreters, who were unable or unwilling to explain to new patients their medical condition, why they had been brought to the hospital and by whom.
When we got to the hospital, we were given a bath and we were shy of our bodies, but I remember being bathed by the nurses that were wearing masks and then they put us to bed. I still can almost hear Inuit crying from being terrified because it was their first time coming into a house that big. Although there were nurses and doctors looking after them, but I can still remember their terrified cries.
Pauloosie Kanayuk, 2005
When patients arrived at the hospital they were given a bath and pyjamas, were escorted to their wards and confined to bed. They were to stay on a strict bed rest until they got better, and were not allowed to touch the floor with their feet (Kay Dier, 2008; Dryden 1985: 94).
I really don’t remember if I was gone for two or three years. I myself think that I was gone for three years because I was in bed for very long time and I didn’t feel sick and since I was in bed for so long I was no longer able to walk. I was even crawling on the floor when they first started to make me walk.
Mary Johnson, 2005
The patients underwent different kinds of treatment depending on where the tuberculosis had affected their bodies. Prior to the availability of antibiotics to treat TB in the late 1940s, Inuit (as well as the general Canadian population) who were sent to hospitals in the South did not receive any medication for their illness. Instead, the treatment in the early days consisted mostly of bed rest, fresh air, surgery, and plenty of protein rich food such as eggs and milk (Grygier 1994: 108-116). It was believed by the medical expertise of that time that by resting the patient allowed the lesions in the lungs caused by the tuberculosis infection to heal and that the fresh air would have a positive impact on the healing process. For exposure to fresh air, the patients were taken outside still laying in their beds, in wheelchairs and even on stretchers (Saskatchewan Lung Association et al. 2008; Wilson 2006: 34-38).
The bed rest routine is well remembered by all the Inuit former TB patients—a routine that would continue even once antibiotic drugs became standard treatment (Thamasie Simarapik, 2008). Patients had to follow a strict routine depending on the stage of their illness. The strictest routines involved complete bed rest and gradually allowed more freedom as the patient recovered from tuberculosis (Dryden 1985: 94). It was difficult for many of the Inuit who were used to an active life outdoors to be confined to bed—particularly the children. In concordance with the accepted treatment for TB at the time, the bed rest routine was strictly imposed on Inuit patients with little understanding of how difficult it was for them to stay in bed. At the Charles Camsell Hospital in Edmonton, sometimes a cast would be placed on both legs of those patients who would not comply with the strict order of bed rest (ibid.: 29-30).
Participants interviewed for this study indicated that being bed ridden for lengthy periods of time, with little understanding of why, was a very challenging aspect of their hospitalisation. How the patients were treated by the medical personnel and other staff seems to have varied across hospitals and time periods. At some hospitals the medical personnel were very strict and would use punishment to make sure that the routine was followed. For example, at Clearwater Indian Hospital in The Pas, if children were caught sitting up in bed during rest periods, their hand would be strapped. If they were caught with a foot on the floor they would be put in straitjacket for up to 24 hours. Markoosie Patsauq related an episode where he was punished for playing with another child during rest period—he was spanked and put in straitjacket for four days (Markoosie Patsauq, 2008). Described in his own words:
The punishment was different types of punishments depending on the kind of things that you did. If during the rest period if I sit up on my bed, which I was not allowed to, I would receive 4 or 5 straps with the ruler. In all those years lot of us were not allowed to step on the floor, like we had to stay in bed. If I put my foot down on the floor […] even just one foot, not both, even just a little step on the floor, and if I get caught I would go down in a straitjacket for the whole day […].
Markoosie Patsauq, 2008
Some participants indicated that children who did not understand French or English would get yelled at for not doing what they were told. Others mentioned that the nurses would patrol the wards with a ruler or a yardstick to hit any misbehaving children. The medical personnel did not normally comfort the children with physical contact such as hugs or hand holding, although treatment provided by nurses and doctors seems also to have depended on their personalities—some were stricter than others while some nurses and children had very positive relationships and grew attached to one another (Imaapik “Jacob” Partridge, 2008; Markoosie Patsauq, 2008; Johanna Rabinowitz, 2005, 2006, 2007).
Arriving at the hospital, Inuit patients were separated depending on gender and age and were sent to different wards. Children were separated from the parents and sent to the children’s ward. In some sanatoriums, such as the Charles Camsell Hospital, patients were required to make a special request to see a family member or friend in another ward, something that was difficult for Inuit patients since often no interpreter was available (Kay Dier, 2007; Dryden 1985: 94).
They could visit. It was a kind of formal process, it wasn’t as good as it should have been, I think. But yes, and husbands and wives sometimes they could visit but they had to kind of put in a request and then you know […]. And I can remember from time to time taking […] you’d take them usually on a stretcher and then take them to the conference room and then they could meet there […]. I think the visiting could have been more generous than it was perhaps.
Kay Dier, 2007
Sometimes patients would feel too shy to ask permission to visit other patients, especially if they did not know any English or French.
We used to write on a piece of paper when we wanted to go to other rooms, just writing down the room number and that’s how we used to communicate. It took me a long time before I was able to ask because I was very shy and was too afraid to ask even to this day I am still little bit like that. When I saw other people writing down on a piece of paper, I started to do it as well.
Lizzie Gordon, 2005
Whether on a strict routine or a more relaxed routine, patients were encouraged to do a variety of activities. Activities were often segregated; men often carved soap stone or painted, while women were encouraged to sew clothing and other similar crafts (Figure 5). These crafts were then sold or given away to important hospital visitors, providing Inuit patients with a form of income. Indeed some of the today’s well known Inuit soapstone artists began their carving at the hospital while being treated for TB (Sarah Ekoomiak, 2007; Grygier 1994: 104-116; Imaapik “Jacob” Partridge 2007; Staples and McConnell 1993; Wilson 2006: 178-181).
Some of the sanatoriums provided a school for the children who were there for extended treatment (Figure 6). Some of the participants indicated that it was at the sanatorium school where they learned to read and write (in English or French) and for a few, this was their first experience at a basic education. At the Mountain Sanatorium in Hamilton, they also had a teacher who taught in Inuktitut. In sanatoriums such as the Mountain Sanatorium and the Charles Camsell Hospital, different trade and university courses were offered to adults who, due to the long-term effects of tuberculosis and surgery, would be unable to return to hunting and fishing (Grygier 1994: 104-116; Wilson 2006: 178-180). Nevertheless, the interviews reveal that the participants’ experiences of the education provided in the hospital were mixed.
Figure 5
A woman sewing a parka in bed at the Mountain Sanatorium in Hamilton.
Figure 6
Children in school at the Mountain Sanatorium in Hamilton.
I think that it was one year after I came to the hospital, I was able to go to school. Right in the hospital. It was maybe five or six of us. And we had one teacher. A little classroom, not bigger than this (pointing around in his office) […] in that little classroom I learnt a lot—how to do the arithmetic and spelling. That really helped me when I started to go to that little school […]. So that wasn’t all that bad after a year in the hospital. I was getting used to the place. I was learning English little more. I was learning about arithmetic and so on […]. I was kind of enjoying it the year after.
Markoosie Patsauq, 2005
They tried teaching us every two weeks and I couldn’t learn anything because it was too hard for me. Although some people were learning, I just couldn’t, but sometimes I’d recognise [a] few words even in French. I can understand little bit, I just don’t know how to speak [it].
Lizzie Gordon, 2005
By the late 1940s, antibiotic drugs had become the accepted cure for tuberculosis. Despite the welcome discovery of an effective cure, treatment and recovery would last months or years, and patients remained in the sanatoriums for extended periods of time. In 1949 at the Mountain Sanatorium in Hamilton where they had begun to treat the TB patients with para-amino-salicylic (P.A.S.) in combination with streptomycin, the average number of days a patient was hospitalised for tuberculosis was 562 days. By 1956, the average stay had decreased to 332 days (Wilson 2006: 160).
Fear and depression as part of daily life at the hospital
Although depression as a concept or diagnosis was virtually unheard of in the 1940s and 1950s, several of the participants indicate that they suffered from depression during their hospital stay, a fact that was also mentioned in interviews with former hospital personnel. In their recall of events at the time, many of the participants suggest that they themselves, as well as other tuberculosis patients on their ward would suffer from depression as a result of worrying about their health, worrying about how their family was coping while they were away, and if they would ever see their home or relatives again (Gale 1979: 81-84; Grygier 1994: 104-116; Pauloosie Kanayuk, 2005).
I was also counselling Inuit who were suffering from deep depression because they thought that they would never go back home. I would counsel the ones that were thinking that they would never see their families again […] No wonder some would get depressed because we sometimes wouldn’t get any news from our relatives for almost up to a whole year. There was no telephone and it was only by mail that we would find out about who had died and we’d also find out that our family members are fine. We’d receive mails anywhere between five and seven months later.
Pauloosie Kanayuk, 2005
Without mentioning depression itself, some of the participants describe feelings of fear and isolation resulting from suffering through their illness and other related tragedies without the support of family or friends.
I was afraid for being in an isolation room where nobody was to stay with me because I had TB and I thought I was never going to get better ever again […]. Nobody explained to me about anything, but I used to pretend to be asleep […]. When I was lying down on my back for couple of hours, my mind would go crazy so, I used to pretend to sleep. There were other Inuit on the same floor, but we were in different rooms. They told us not cross the lines on the floor to prevent others from catching the TB infection. I had to wear a mask all the time. At that time I didn't know I was pregnant and I was taking medications and needle shots every day, so the baby I carried got disorders.
Maggie Aqiaruq Aliqu, 2005
The TB patients sometimes kept in touch with their families in the North by writing letters in Inuktitut. Both TB patients and family members in the North would also write to government authority figures to ask for assistance in finding family members or having them returned (Grygier 1994: 129-130; Tester et al. 2001). However, the mail was very slow between the North and South of Canada, since it was transported with the Eastern Arctic Patrol or the Canadian Air Force (Imaapik “Jacob” Partridge 2007; Markoosie Patsauq 2005). Separation from family, struggling with illness, and the loss of family members to tuberculosis, whether through separation or death, must have contributed to the emotional state of the Inuit patients.
Once their health had improved, some Inuit patients took on responsibilities at the hospital acting as informal, unpaid social workers. Some would visit other Inuit patients and try to lift their spirits while others would translate for patients and medical personnel in order to alleviate the confusion that resulted from being unable to communicate with their doctors and fellow patients (Pauloosie Kanayuk, 2005; Sarah Ekoomiak, 2007).
Returning home…
Well it took me a couple of years to realise that I needed to pick up my language. Before two years while I was home I thought no I don’t need to learn it because there’s English.
Imaapik “Jacob” Partridge 2007
Interviews with Inuit former tuberculosis patients indicate great variation in the ways that individuals adjusted to their hospital stay and their return to life in the North. While some adjusted well to the hospital stay and found it relatively easy to reintegrate with their home communities due to their retention of Inuktitut and other Inuit skills, other interviewees found their adjustments more challenging.
The other side of me wanted to go back to Hamilton because I was there for three years. The dogs were loose all over the place and I thought I was going to be attacked by them. As the days went by one day at a time, I started getting used to it again. During the summer I used to mostly stay in the water a lot to keep myself clean. I didn’t like getting close to my relatives because I thought they’d pass on their head lice. I would worry about using the same cup that my family members were using because I learned at the hospital how to prevent from getting bacteria.
Pauloosie Kanayuk, 2005
Pauloosie Kanayuk found it challenging to adjust again to the cultural habits of the Inuit. He felt particularly insecure about not having regular mealtimes—he never knew if his family was going to eat together or when they might eat. Yet, he indicates that his family helped to ease this period of readjustment by trying to change some of their own habits, for example, by washing the blankets more often to make him more comfortable regarding his concerns with hygiene.
For those who were very young when they went to the hospital, it was difficult to return to their home community since they had learned either English or French at the hospital and forgotten much of their Inuktitut. Some could no longer speak or understand Inuktitut and had problems communicating with their parents. Others had been sent to the hospital at such a young age that they did not recognise their parents when they returned and instead wanted to stay with the nurses (Figures 7 and 8) (Johanna Rabinowitz, 2005, 2006). Those who were sent to sanatoriums in Quebec had learned French and when they returned they were often then placed in English schools (since all the schools were run by the federal government). As a result these children were forced to struggle with both English and Inuktitut (Grygier 1994: 125). Depending on the length of stay at the hospital, many of the children and youth had lost their traditional skills, such as hunting and sewing, or in the case of those who had left at a very young age, had never acquired them. Children who returned home after a lengthy stay away had to begin a learning process to reclaim these abilities. Skills such as language, sewing and hunting were important to master not only for survival but also as outward proof of Inuit identity. Imaapik “Jacob” Partridge indicated that his family acknowledged his behaviour as different from the behaviour of other Inuit children.
[T]hey didn’t know anything about white men other than the clothes, you know. Like I didn’t act like a white man there, but I had some differences from the other children.
Imaapik “Jacob” Partridge, 2007
The return to their home communities was an adjustment that took time, yet was successful for many of the former tuberculosis patients. Several of the participants indicated that the retention of traditional cultural skills such as speaking Inuktitut and subsistence practices such as hunting, fishing and making bannock made the readjustment a relatively easy one.
I could still speak my own language. I had been to the Resolute before. I stayed with my family. So it wasn’t hard to get used to coming to that life again
Markoosie Patsauq, 2005
I didn’t mind about the difference of the food, after all I was still an Inuk. I didn’t forget how to make bannock and I had no problem adjusting back to my home
Mina Qilurqi Matt, 2005
I still remembered, so I knew what do to.
Mary Johnson, 2005
Figure 7
Children about to begin their journey back to their home community in the North, at the Mount Hope Airport, Hamilton.
Figure 8
Three girls, tagged with name, disk number, and home community name, about to board the plane at the Mount Hope Airport, Hamilton.
Several of the participants interviewed indicated that it was difficult to re-adjust to the Inuit way of life after having been at the hospital for so long. Upon returning home, many had a hard time returning to sleeping in an igloo or tent, especially when they had not completely recovered from tuberculosis or the effects of surgery. Still others found that habits they had adopted at the hospital such as eating meals at regular times, and strict adherence to hygiene made their return home, where they could not always follow these new habits, a stressful experience. In addition, many of the former tuberculosis patients had left home at such a young age, and had been gone for so long that they had lost much of their cultural knowledge. Upon their return, they were questioned by the other Inuit who found their behaviour strange or typical of Qallunaat.
Everything was difficult because I didn’t know how to adapt. My older sister used to ask me why I was acting the way I did. She used to say; “Are you now a Qallunaaq?” Even before I left for the hospital I used to sew a lot and when I came back I tried doing the same thing but, I was getting mad at for not sewing properly and what I sewed would even be ripped and me doing it all over again. I thought I was doing okay. I was told; “that's not how you do!” So, that was really hard for me.
Lizzie Gordon, 2005
It was not only those who went away to the hospital who experienced change. When these former tuberculosis patients returned to their home communities after months or years away, they returned to communities which had gone through many transitions; people had started to move into houses, children had started to attend school, and some people were wage earners (Dorais 1997; Patrick 2003: 92-97).
I remember big changes like people going out at night like they never used to do before I left. They went out to go see movies when the Catholic missionaries had come here in Puvirnituq. It was as if [I] came back home to a strange home when I came back because they had changed so much.
Mary Johnson, 2005
In 1945, the government began providing a family allowance to Inuit families. Beginning in the 1940s, schools were being built by the Canadian government in communities in northern Quebec and in the Northwest Territories, and by 1961 there were schools in most Inuit communities (Jenness 1972: 77-79). To be eligible for the family allowance, the children’s attendance at school was mandatory. In order to allow their children to stay at home, rather than being sent away to boarding houses, many Inuit began to move into communities (Wachowich 1999: 107-110).
Negotiating identities as a form of resilience
While not everyone belonging to a given cultural group displays the same behaviours, values and skills, there exist certain characteristics that members of a cultural group learn as they grow up, characteristics which are often essential for the survival of the individual within that culture (Keesing 1994; Kurkiala 1997, 1998). Among Inuit in the 1950s, language and certain skills such as hunting and trapping (for men) as well as preparing food, sewing clothes, and taking care of the children (for women) were identified by participants as important in their ability to transition back to their lives in Inuit communities following a lengthy hospital stay. Inuit who went to the hospital for treatment had to learn other behaviours, skills and values that were typical of Euro- Canadian culture of that time. Upon returning to their home communities, they faced challenges to their identity, both in terms of their re-adaptation to Inuit life and in terms of the manner in which they were perceived by family and the community as a whole.
Following the work of Olofsson (2004) on ethnic identity and building on the theories of Anthony Cohen (1995: 56-65) and Mikael Kurkiala (1998), we make a distinction here between the “ethnic labelling” of an individual from the actual experience of identity—the self-experienced identity. A person can choose to take on an “official” ethnic identity as Inuk for a variety of purposes, such as checking a box for a census, yet at the same time hold a fluctuating, fluid self-identity that adjusts according to cultural context and personal circumstances. For instance, an Inuit identity can become stronger living among other Inuit persons. Or, an individual can feel that she is no longer like the others of her ethnic group since she has changed in behaviour and values, but nevertheless, she may continue to label herself as a member of that ethnic group, as in this case, Inuk. Likewise, others of the same group may feel that an individual is acting out of the ordinary for a member of their ethnic group; however, they might still label her as Inuk. In addition, how an individual defines his or her identity might differ from how others of that cultural group might define that individual’s identity; for example, a person can consider himself or herself to be Inuk but might not be considered Inuk by everybody else.
According to our interviews, the experience of leaving one’s family, living in the hospital, being subjected to hardship, exposed to other cultures and taking up different cultural skills, behaviours and values did not permanently change the self-identification of the Inuit evacuees participating in our study. They continued to perceive themselves as Inuit, despite having “lost” cultural knowledge associated with “being” Inuk. Rather, we argue that the cultural knowledge acquired during their hospital stays could instead be considered as supplementary to their individual identity. While factors determining an individual’s re-integration with their home community appear from the interviews to be related to the retention of Inuit cultural skills, such as language, sewing, and hunting; the inability to readjust to Inuit life should not be perceived as “losing” Inuit identity or of “becoming” Qallunaaq. Rather, as indicated by several of the participants, learning the skills or practices of another culture or having to re-learn the skills of Inuit culture did not compromise the individual’s identity, but contributed to the individual’s ability to adapt their identity. As we have shown here, those interviewed for the study negotiated and integrated the skills, behaviours and values learned during their hospital stays with the skills, behaviours and values of their Inuit identity regardless of whether they chose to live in an Inuit community or in other areas of Canada.
These former TB patients demonstrate resilience in the face of extremely challenging situations. As young adults and children ill with tuberculosis, relocated away from home and provided little communication with family, these individuals were able to adapt to the hospital environment each in their own way. After a lengthy time away, these participants then either re-adjusted to their home communities, or chose to make homes for themselves in the south of Canada, all the while, maintaining their identity as Inuit. Thus, the concept of an Inuit identity must be understood as fluid, holding different meanings for different individuals, and liable to change and evolve over time and place.
The psychological concept of resilience has changed over time as well, from an understanding of resilience as an exceptional quality toward the view of resilience as a natural part of an individual’s developmental process in interaction with their social and cultural surroundings (Luthar et al. 2000). One exception to this change is the resilience literature surrounding Aboriginal peoples, where resilience is not viewed as such a process, but instead continues to focus on the individual’s psychological traits (Holton et al. in press). The concepts of culture and resilience have been reified in the literature surrounding “Aboriginal resilience” and are defined as unchangeable and constant concepts. According to Holton et al. (in press), Aboriginal culture in this context is problematically seen as a hands-on tool to educate individuals to become “resilient Aboriginal individuals.” This reification of “Aboriginal resilience” as an individual characteristic, allows for the challenges faced by Aboriginal peoples to be located at an individual level rather than at a societal and political level. Responsibility for change then falls to the individual. Further, the perception of culture as a tool that bestows resilience upon the individual allows for the possibility of exclusion based upon who possesses traditional culture and who does not (ibid.).
In contrast to this view, we argue that the concept of culture and its related concepts of ethnic identity and ethnicity are changeable, and that one person’s ethnic identity can be influenced by elements from different cultures without losing his or her belonging, and without compromising resilience. Culture does not equip one with a standard identity but instead offers resources for developing many, fluid, hybrid identities by means of social positioning and narrative constructions of the self (Bhabha 1994). Instead of viewing Aboriginal culture as necessarily static for the health, belonging and wellbeing of an individual, we have shown here that the human capacity of “culture crossing” and borrowing from other cultures is an important coping mechanism and a form of resilience in and of itself.
Conclusion
The narratives of these former tuberculosis patients are not merely illness narratives. They are also narratives about living and coping in different cultural contexts and of how this experience affected their identity, both as they perceive themselves, and as they are perceived by others. Their narratives indicate that a variety of factors aided in the ability to negotiate identity and adapt in the face of adversity. At the hospital, some of the factors that helped these individuals to cope included: the ability to easily learn other languages and hence to communicate with medical personnel and other patients, the ability to easily form relationships, as well as the opportunity to participate in meaningful activities, such as schooling, professional courses and work, such as carving and crafts. Adjusting to the return home was eased for those who had a supportive family willing to accept and adjust to the changes of their family member, and to adopt some of their family member’s new habits. The retention of Inuktitut, of cultural knowledge or the ability to re-learn these skills were mentioned as factors by those who were able to reintegrate well in their home communities.
In retelling the stories of Inuit former tuberculosis patients, we have discussed notions of culture and individual ethnic identity. We have illustrated in this article how individual ethnic identity fluctuates with immersion in another culture. These narratives are also part of a larger, societal narrative regarding Inuit, the rest of Canadian society, the relationship between the two societies and the changes that occurred from the 1940s to the 1960s. We call into question the notion that the definition of Inuit must fill certain criteria and instead have demonstrated how being Inuit can mean different things to different individual Inuit and may fluctuate over time according to a variety of aspects such as cultural context and living conditions. The experience of being taken from their families, of adjusting to a new culture and to hardship due to illness and treatment at the hospital, and adapting to their return home had no influence on their self perception as Inuit. While their ethnic identity straddled two or more cultures, influenced by years away from their home during formative times in their lives, the individuals in this study demonstrate resilience, not only in their ability to cope with change and hardship, but in the retention of their self-identification with Inuit, despite how others perceived them. They remained Inuit, and adapted new aspects of their ethnic identity into the life they chose to lead after their hospital stay. As Lizzie Gordon indicates, she did learn how to sew again. Better than her sister.
Parties annexes
Acknowledgements
Our sincere thanks to Johanna Rabinowitz, Shawn Selway, Bob Mesher, and all the interviewees who shared their stories and gave their kind permission to use them. This research was funded by the Fonds québécois de la recherche sur la société et la culture; the National Network for Aboriginal Mental Health Research; the Culture and Mental Health Research Unit of the Jewish General Hospital (Montreal); the Avataq Cultural Institute; and “Roots of Resilience: Transformations of Identity and Community in Indigenous Mental Health” of the Canadian Institutes of Health Research.
Notes
-
[1]
Qallunaaq is the Inuktitut word for a non-Inuit individual of European heritage. Qallunaat is the plural form (George Filotas, pers. comm. 2008).
-
[2]
Starting in the 1940s, numbers were assigned to the Inuit by the Canadian Government which were engraved on small disks for each individual to wear (Alia 1994: 32-39).
-
[3]
This is a pseudonym.
Bibliographie
- Maggie Aqiaruq Aliqu, 2005
- Kay Dier, 2007
- Maggie Ekoomiak, 2007
- Sarah Ekoomiak, 2007
- George Filotas, 2008
- Lizzie Gordon, 2005 (interviewed by Mélissa Solokoff)
- Mary Johnson (pseudonym), 2005
- Pauloosie Kanayuk, 2005
- Imaapik “Jacob” Partridge, 2007, 2008.
- Markoosie Patsauq, 2005, 2008.
- Johanna Rabinowitz, 2005, 2006, 2007.
- Thamasie Simarapik, 2008
- ALIA, Valerie, 1994 Names, Numbers, and Northern Policy, Halifax, Fernwood Publishing.
- BHABHA, Homi, 1994 The location of culture, New York, Routledge.
- BRODY, Hugh, 2000 The Other Side of Eden: Hunters, Farmers, and the Shaping of the World, Vancouver and Toronto, Douglas and McIntyre.
- COHEN, Anthony P., 1995 Self Consciousness. An Alternative Anthropology of Identity, London and New York, Routledge.
- DORAIS, Louis-Jacques, 1997 Quaqtaq: Modernity and Identity in an Inuit Community, Toronto, University of Toronto Press.
- DRYDEN, Donna (ed.), 1985 The Camsell Mosaic: The Charles Camsell Hospital, 1945-1985, Edmonton, Charles Camsell History Committee.
- DUFFY, Quinn, 1988 Road to Nunavut. The Progress of the Eastern Arctic Inuit since the Second World War, Kingston and Montreal, McGill-Queen’s University Press.
- GALE, Godfrey L., 1979 The Changing Years: The Story of Toronto Hospital and the Fight Against Tuberculosis, Toronto, West Park Hospital
- GRYGIER, Pat Sandiford, 1994 A Long Way from Home the Tuberculosis Epidemic among the Inuit, Montreal, McGill-Queen’s University Press.
- GRZYBOWSKI, S., K. STYBLO and E. DORKEN, 1976 Tuberculosis in Eskimos, Tubercle, 57(4 suppl.): S1-58.
- HOLTON, Tara, Gregory BRASS and Laurence KIRMAYER, in press The discourses of resilience, ‘enculturation’ and identity in Aboriginal mental health research, in T. Teo, P. Stenner, A. Rutherford, E. Park and C. Baerveldt (eds), Varieties of theoretical psychology: International philosophical and practical concerns, Toronto, Captus Press: 194-204.
- JENNESS, Diamond, 1972[1964]Eskimo Administration II Canada, Montreal, Arctic Institute of North America Technical Paper, 14.
- KEESING, Roger, 1994 Theories of Culture Revisited, in Robert Borofsky (ed.), Assessing Cultural Anthropology, New York, McGraw-Hill.
- KURKIALA, Mikael, 1997 “Building the Nation Back Up”: The Politics of Identity on the Pine Ridge Indian Reservation, Uppsala, Acta Universitatis Upsaliensis, Uppsala Studies in Cultural Anthropology, 22.
- KURKIALA, Mikael, 1998 Modernity, Culture, and the Construction of Identity, in Alf Hornborg and Mikael Kurkiala (eds), Voices of the Land: Identity and Ecology in the Margins, Lund, Lund University Press.
- LONG, Richard, 2000 Nonrespiratory (Extrapulmonary) Tuberculosis (Chapter II-D), Ottawa, Canadian Tuberculosis Standards 5th Edition, Health/Santé Canada and The Lung Association/L’Association pulmonaire.
- LUTHAR, Suniya, Dante CICCHETTI and Bronwyn BECKER, 2000 The Construct of Resilience: A Critical Evaluation and Guidelines for Future Work, Child Development, 71(3): 543-562.
- MARCUS, R. Alan, 1995 Relocating Eden: The Image and Politics of Inuit Exile in the Canadian Arctic. Hanover, and London, University Press of New England.
- OLOFSSON, Ebba, 2004 In Search of a Fulfilling Identity in a Modern World: Narratives of Indigenous Identities in Sweden and Canada, Uppsala, Uppsala University, DICA Series (Dissertations in Cultural Anthropology).
- OLOFSSON, Ebba, 2007-2008 The story of Markoosie Patsauq’s trip to the sanatorium in The Pas, Makivik Magazine, 83: 18-23.
- PATRICK, Donna, 2003 Language, Politics, and Social Interaction in an Inuit Community, Berlin, Mouton de Gruyter.
- PHILLIPS, R.A.J., 1957 The Eastern Arctic Patrol, Canadian Geographical Journal, May: 190-201.
- SASKATCHEWAN LUNG ASSOCIATION et al., 2008 Canada's Role in Fighting Tuberculosis Web site, http://www.lung.ca/tb/tbhistory/
- SMITH, Derek, 1993 The emergence of “Eskimo status”: An examination of the Eskimo disk system and its social consequences 1925-1970, in Noel Dyck and James Waldram (eds), Anthropology, Public Policy, and Native Peoples in Canada, Montreal and Kingston, McGill-Queen’s University Press: 41-74.
- STAPLES, Annalisa R. and Ruth L. McCONNELL, 1993 Soapstone and Seed Beads. Arts and Crafts at the Charles Camsell Hospital, a Tuberculosis Sanatorium, Edmonton, Provincial Museum of Alberta Special Publication, 7.
- TESTER, Frank James, Paule McNICOLL and Peter IRNIQ, 2001 Writing for our lives: The language of homesickness, self-esteem and the Inuit TB ‘epidemic’, Études/Inuit/Studies, 25(1-2): 121-140.
- VANAST, Walter J., 1991 ‘Hastening the Day of Extinction’: Canada, Québec, and Medical Care of Ungava’s Inuit, 1867-1967, Études/Inuit/Studies, 15(2): 55-84.
- WACHOWICH, Nancy, 1999 Saqiyuq. Stories from the Lives of Three Inuit Women, Montreal, McGill-Queen’s University Press.
- WHERRETT, George Jasper, 1977 The Miracle of the Empty Beds: A History of Tuberculosis in Canada, Toronto, University of Toronto Press.
- WILLIS, John, 1956 John Willis "Eastern Arctic 1956 Summer Survey", unpublished report, Ottawa, Department of Health and Welfare.
- WILSON, Ralph Holland, 2006 Chedoke – More Than a Sanatorium. A Story of Compelling Characters and Changing Times, Hamilton, Hamilton Health Sciences and Altona, Friesens Corp.
Personal communications and interviews
References
Liste des figures
Figure 1
Map showing the hospitals and sanatoriums used for TB in Canada.
Figure 2
People waiting in line for medical examination on board the C.D. Howe.
Figure 3
Markings on the hands.
Figure 4
A child and an elder woman in bed on board the C.D. Howe.
Figure 5
A woman sewing a parka in bed at the Mountain Sanatorium in Hamilton.
Figure 6
Children in school at the Mountain Sanatorium in Hamilton.
Figure 7
Children about to begin their journey back to their home community in the North, at the Mount Hope Airport, Hamilton.
Figure 8
Three girls, tagged with name, disk number, and home community name, about to board the plane at the Mount Hope Airport, Hamilton.