Résumés
Summary
Humans harbour a variety of pathogens that are often transmitted from other animal species. A few are localized in tropical areas, but most enteric pathogens are present everywhere on the planet and they travel with their hosts to distant locations. Several of these microorganisms are transmitted by water that has been contaminated by fecal matter, whereas some are normally found in water but, given an opportunity, will cause disease (i.e., opportunistic pathogens). While waterborne outbreaks have been reported for many pathogens, assessing the proportion of the disease burden to a specific route and pathogen has proven quite elusive. Surveillance of disease in populations, even when actively done, is very inaccurate as it often gathers data on the most acute cases that are only a very small proportion of the true number of infected individuals. There are several issues discussed herein, focusing on the needs and gaps linked to waterborne pathogen monitoring. The benefits and weaknesses of current and emerging methodologies are discussed, in addition to the appropriateness of allocating resources to waterborne pathogen monitoring. The most critical gap is the lack of validation of most methods used in environmental microbiology for the detection of pathogens. Data generated by various laboratories are currently extremely difficult to compare and cannot serve as the basis for risk assessment or management. The issue of laboratory capacity is also raised, within the context of the availability of trained personnel, the application of QA/QC protocols, and accreditation on a national level. In closing, needs are identified for informed communication of the risks of waterborne pathogens, the training of highly qualified personnel, and the development and standardization of methods that will ultimately enhance water safety and public health protection.
Résumé
De nombreux microorganismes pathogènes entériques affectent l’homme et certains peuvent être acquis d’autres espèces animales. Certains sont spécifiques aux régions tropicales, mais la plupart des microorganismes entériques sont les mêmes partout sur la planète, voyageant avec leurs hôtes aux coins les plus reculés. Ils se retrouvent dans l’eau contaminée par les matières fécales excrétées. D’autres sont indigènes au milieu hydrique et sont des opportunistes, causant la maladie chez les individus susceptibles. Par la surveillance des épidémies associées à l’eau, on a pu facilement identifier ceux qui sont importants en santé publique. Il est cependant beaucoup plus difficile d’attribuer quelle part du fardeau de la maladie peut être attribuée à une voie d’exposition spécifique. La surveillance de la maladie dans les populations, même lorsqu’elle est active, est très imprécise puisqu’elle ne collige que les données sur les cas les plus graves, soit une faible partie du nombre réel d’individus infectés. À des fins de santé publique, il y a plusieurs aspects, incluant des besoins et des manques, associés au suivi des microorganismes pathogènes dans l’eau. Les bénéfices et faiblesses des méthodes courantes et émergentes doivent être présentés dans un contexte d’appropriation de ressources au suivi des microorganismes pathogènes dans l’environnement. Le simple fait de vouloir analyser des échantillons pour y détecter des microorganismes pathogènes implique des éléments que trop de chercheurs connaissent mal. Les conséquences publiques, légales, politiques et économiques ont été mises en évidence lors de plusieurs événements partout dans le monde, mais plus récemment à Sydney en Australie. Une erreur de laboratoire a conduit à la détection (fausse) de parasites (Cryptosporidium) dans l’eau potable : cette erreur a coûté plus de 37 millions de dollars et affecté trois millions de résidents sans qu’aucune infection ne soit observée. Les producteurs d’eau veulent connaître le niveau de pollution de leur eau d’approvisionnement afin de déterminer le niveau approprié de traitement : comme les méthodes sont imprécises, la marge d’erreur est très grande. Les recommandations présentes sont plutôt dirigées vers des paramètres physico-chimiques (turbidité, mesure de désinfectant en continu, etc.) et des plans de sécurité lesquels sont facilement applicables, mesurables et fiables.
Les méthodes actuelles de détection des microorganismes pathogènes sont peu fiables et leur diversité dans les différents laboratoires rend l’interprétation difficile. Le manque le plus important reste le peu de validation de la plupart des méthodes de détection des microorganismes pathogènes en microbiologie environnementale. Les données fournies par des laboratoires différents ne peuvent donc être facilement comparées et ne peuvent servir à faire des évaluations de risque ou de la gestion de risque. En général, peu de laboratoires offrent de telles analyses, le personnel qualifié est rare, les protocoles de QA/QC sont rarement présents et il n’y a aucune accréditation nationale. La formation de personnel hautement qualifié et le développement de méthodes standardisées ne pourront donc ultimement que mieux servir la santé publique. Les méthodes actuelles utilisées dans un cadre bien défini de certains projets de recherche écologiques commencent à porter fruit. Les données de positionnement géographique, climatologiques et microbiologiques doivent être évaluées afin que la qualité des données produites par les modèles écologiques soit valide. En résumé, les informations acquises sur la présence des microorganismes pathogènes dans les eaux de surface sont utiles mais ne peuvent être utilisées que si elles sont validées. Les laboratoires effectuant les analyses devront être accrédités et devront utiliser des méthodes standardisées si nous voulons comparer les données fournies. Ce n’est qu’à ce moment que l’analyse quantitative du risque microbiologique pourra se faire. Cette nouvelle approche est en émergence au niveau international et les modèles proposés doivent utiliser des données précises. Au Canada, l’Agence de santé publique du Canada s’intéresse à cette nouvelle approche. En l’absence de mesures précises, les chercheurs et les agences de contrôle doivent utiliser les indicateurs de traitement et de contamination fécale pour s’assurer de l’innocuité de l’eau de consommation. Alors que les protocoles d’analyse sont bien définis pour ces paramètres, ceux requis pour les microorganismes pathogènes ne sont pas encore établis. Or, des analyses occasionnelles ou mal ciblées ne sont pas valides pour des fins de santé publique.
Les organisations internationales, telles l’Organisation pour la coopération et le développement économique (OCDE) et l’Organisation mondiale de la santé (OMS), s’intéressent aux méthodes récentes qui allient la biologie moléculaire et la bioinformatique pour obtenir des réponses rapides et fiables sur la contamination des eaux. Ce sera par l’éducation et la communication que les risques pourront être établis et que nous pourrons en informer correctement le public en général, la communauté scientifique, les agences gouvernementales et les producteurs d’eau. Les recherches futures devront répondre aux questions de méthodologie, sensitivité, spécificité, et surtout aux questions de valeur prédictive des résultats de détection de microorganismes pathogènes.
Corps de l’article
1. Waterborne Pathogens
Pathogens of public health significance are found in ambient water almost everywhere. Some of these pathogens have been excreted in the environment by an infected human or animal host. Others are opportunistic pathogens that are part of the normal water biota, but, when given the opportunity to infect a human host, can cause disease.
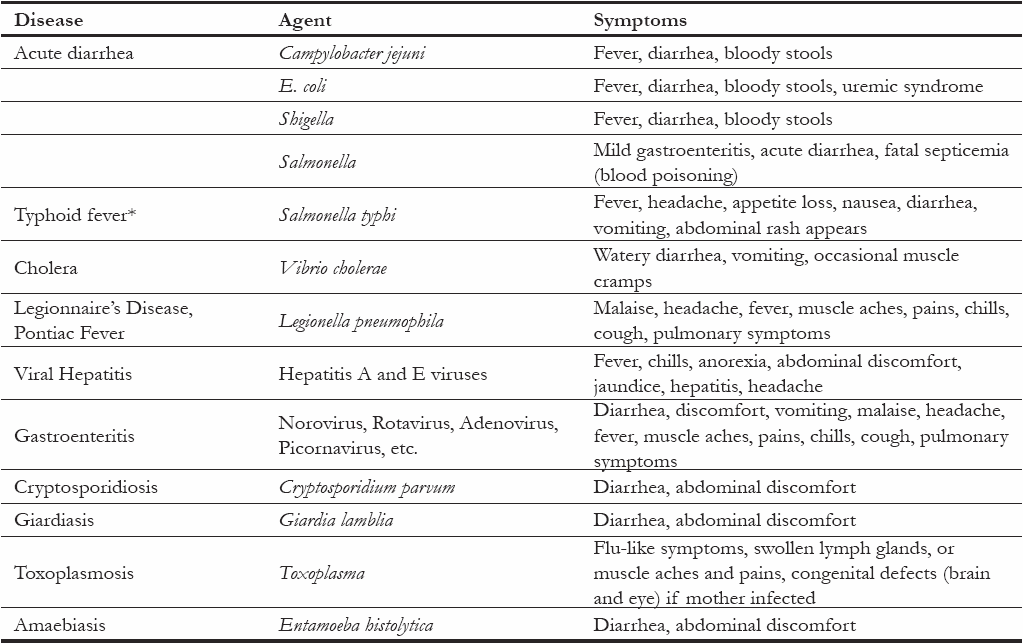
Most waterborne pathogens are well described as they have been implicated in numerous waterborne outbreaks worldwide (ANON, 1999; HURST et al., 2002; WHO, 2006). The diseases associated with waterborne pathogens can affect any organ of the human body and they are often described by the symptoms associated with the infection (e.g., diarrhea, gastroenteritis, pneumonia, hepatitis, meningitis, etc.) (Table 1) (WHO, 2006). Human enteric viruses present a particular challenge because viral infection often results in non-specific symptoms that can be respiratory, gastrointestinal, neurological, cardiovascular, ocular or dermatological (HEYMANN, 2001). However, when they reach a target organ, they can produce severe disease (poliomyelitis, hepatitis, meningitis, diabetes, myocarditis, etc.) (Table 2).
Table 1
Diseases, agents and symptoms associated with waterborne disease (data from HeymanN 2001).
Maladies, microorganismes et symptômes associés aux maladies transmises par la voie hydrique (données modifiées de Heyman 2001).
Table 2
Diseases and syndromes associated with enteric viruses.
Maladies et syndromes associés aux virus entériques.
In addition to the microorganisms listed in table 1, emerging pathogens present a new level of risk to public health. With increasing human travel (both in frequency and speed) between countries, most pathogens are continuously circulated internationally and can therefore be considered a hazard everywhere that they can survive: infected individuals, symptomatic or not, become the transportation vehicles. The full impact of this was evident in the recent global SARS outbreak of early 2003, which involved a rapid worldwide spread of this new pathogen to five continents and 30 countries, demonstrating the potential threat an infectious disease poses in the new global public health community (WHO, 2003b).
It should be assumed that the human population is exposed to most known waterborne pathogens and that the level of exposure is a function of hygiene, sanitation and water treatment. Furthering the understanding of the mechanisms through which pathogens emerge is critical to the delivery of safe drinking water and the protection of public health. However, the level of risk from emerging pathogens must be balanced, evaluating the perceived risk of an emerging disease with true public health risk reality — sometimes the ends of the spectrum are so far removed that inappropriate allocations of resources are committed towards these issues (HRUDEY and LEISS, 2003; WHO, 2006).
2. Water As a Route of Exposure
Most pathogens of human importance are transmitted by the fecal-oral route; water is only one of the many vehicles through which they are disseminated in the environment (ANON, 1999, HURST et al., 2002, PAYMENT and RILEY, 2002). Food, air, and contact with other individuals, inanimate objects, pet or farm animals, and soil are all potential routes of exposure or vehicles of transmission.
From epidemiological data on reported cases of disease in industrialized countries, it is understood that personal contact is the main route of transmission, followed by food, water and other sources (HUNTER, 1997; HUNTER and FEWTRELL, 2001). The number of reported cases of disease is a poor estimation of the magnitude of these infections. It is estimated that, for every case reported in Canada through the current notifiable disease system, there are approximately 314 cases of infectious gastrointestinal disease in the community (MAJOWICZ et al., 2004). Studies from other developed countries have reported that about 15% to 30% of acute gastroenteritis cases consult a physician and as many as 4% are hospitalized (WHEELER et al., 1999; KUUSI et al., 2003, SCALLAN et al., 2004). It is clear that the burden of enteric disease remains substantial in developed countries.
It is unfortunate that, in reference to the infectious disease reporting, any link between pathogen and water as the route of transmission is rarely addressed (PAYMENT and RILEY, 2002). The global level of disease transmitted by water is most often estimated through the monitoring of outbreaks and targeted epidemiological studies. Recent reviews of the microbial safety of water have been prepared by the World Health Organization (FEWTRELL and BARTRAM, 2001; WHO, 2006), the American Academy of Microbiology (PAYMENT and RILEY, 2002) and the Organization for Economic Cooperation and Development (DUFOUR et al., 2003). These reviews collectively conclude that in most countries outbreak reporting is at best poor and that the relative importance of each transmission route is essentially unquantifiable at this time. Some progress has been made in Denmark and the United States with respect to attributing levels of gastrointestinal illness to specific foods, but the waterborne route of transmission is, as of yet, excluded from these analyses (HALD et al., 2004; BATZ et al., 2005).
It is understood that there are major differences related to disease transmission in an urban versus an agricultural context. In an urban environment, personal contact is probably the major route of transmission. In an agricultural environment, exposure to animals and their excreta certainly play a very important role in the transmission of pathogens. Exposure to water in agricultural settings should also be considered separately from water in an urban setting; most drinking water is obtained from groundwater wells that are less regulated and often contaminated in agricultural communities or private residences. In the US, most drinking water outbreaks have been associated with untreated groundwater, especially from private wells (CRAUN, 1992; LEE et al., 2002; FROST et al., 2002). In the UK, a recent report indicated that although private water systems only serve 0.5% of the population, 36% of drinking water outbreaks were associated with those private water supplies (SAID et al., 2003).
Determining the mode of pathogen transmission and the respective contribution of each route of exposure is considered a moving target since the incidence of disease can vary by a factor of 10 over time, within a year and between years (PAYMENT and RILEY, 2002; PAYMENT et al., 1997). Unfortunately, for the majority of enteric disease cases in Canada, neither the pathogen nor the source of transmission is identified (Lee, 2003).
Most studies indicate a mode of transmission and incidence at a local level, but they cannot be uniformly applied to obtain a national picture. The total incidence of gastrointestinal disease in industrialized countries has been estimated at 0.5 to 1 episode per person-year and Canadian epidemiological studies have reported rates of gastrointestinal illnesses at a level of about 0.7 episode/person-year. A recent Health Canada study reported an incidence of roughly 1.3 case of enteric disease per person each year in Canada (MAJOWICZ et al., 2004). In the late 90s, two Canadian studies suggested that 35 to 50% of gastrointestinal illness cases were associated with treated drinking water that met Canadian drinking water guidelines (PAYMENT et al., 1997). A similar study in Australia (HELLARD et al., 2001) and a recent US study (COLFORD et al., 2005) have not identified waterborne disease associated with drinking water meeting national regulations.
Regardless of the need for addressing emerging issues related to waterborne pathogen transmission, there is a concern that scientists across the disciplines still do not understand the basic issue of waterborne disease transmission, and are not correct in their interpretation of the knowledge that currently exists regarding the importance of water as a pathogen exposure route.
There is a need in Canada, as in all countries, to create a network of researchers and public health authorities to better understand the role of water in the transmission of enteric and respiratory diseases, by improving the quality and quantity of data collected to inform water safety and public health decision-making.
3. Pathogen Monitoring
Waterborne pathogen monitoring is an intricate issue. Whether or not pathogen monitoring of source or treated drinking waters is required has been the subject of heated discussions in the literature (ALLEN et al., 2000; PAYMENT et al., 2003). Experiences in other countries have shed some light on the public, political, economic and legal implications of positive pathogen results in treated drinking water in the absence of any detectable health effects in the population. In 1998, a series of water safety scares occurred in Sydney, Australia, with three successive episodes of «boil water» notices affecting up to three million residents. The apparent detection of Cryptosporidium oocysts in the treated water supply cost the city and its taxpayers over 37 million $ in direct costs, although no evidence of an increase in gastrointestinal disease in the community was established and the water sample results were ultimately attributed to improper laboratory procedures (HRUDEY and HRUDEY, 2004). These cases show that, unless it is known how to interpret the results and an emergency plan is in place to react to a positive result, the subsequent response protocols may be inappropriate.
From a research point of view, gathering knowledge on pathogens in the environment is an integral part of the scientific process. As emerging pathogens (WHO, 2003a) are identified, the methods are developed for their detection and identification in various samples such as biological material, water, food and soil. In addition, data obtained by researchers provide useful information on various parameters that can be used as indexes, indicators or surrogates for waterborne pathogens (ANON, 1999).
From a water utility perspective, information on the occurrence of waterborne pathogens in the source water is useful to insure that they are not present or are effectively removed by the treatment process. However, water is treated because we assume it needs treating. Knowledge of the level of pathogens in the source water is not essential to the provision of safe drinking water at a treatment plant — what matters in terms of protecting public health is that the water is treated, a residual is maintained in the distribution system and that the design and operation of the water treatment plant incorporate sufficient levels of barriers and control to reduce the risk to the community.
Because of the lack of real-time, validated monitoring methods for waterborne pathogens or indicators, test results for water collected immediately following treatment (prior to distribution to the community) essentially provide results for water that has already been consumed. Thus, the provision of safe drinking water should not merely focus on the monitoring of pathogens, due to the time lag between the collection of a sample, the associated test result, and the public consumption of the treated water before the test result is obtained. Microbial water quality can often vary rapidly, and timely dissemination of microbial testing of water is often not available in time to inform decision-making processes at the water utility or public health unit (WHO, 2003b). An important component of the public health protection mandate is to know, in real time, that the distributed water is safe, through treatment parameters such as turbidity and disinfectant residual, rather than direct pathogen monitoring. Low turbidity levels in treated drinking water appear to offer significant removal benefits for protozoans and appropriate disinfectant contact time provides microbiologically safe drinking water (USEPA, 2003).
Therefore, emphasis must be placed on public health protection through the development of source-to-tap water safety plans, or quality management frameworks, that address hazards in the system and provide mechanisms for appropriate treatment plant operations (and training), monitoring, and communication (WHO, 2006; NHMRC, 2004).
The need does occasionally arise to directly monitor for pathogens in treated water to identify the source of exposure, when an outbreak occurs and epidemiological data suggests the route of transmission is waterborne. However, methods to detect the causal agent in waterborne outbreaks are typically inefficient at identifying the source (WHO, 2006).
Data on the occurrence and risk of waterborne pathogens are the basis for the regulatory development process and associated risk management initiatives. For example, in the UK water utilities process thousands of samples per year to detect Cryptosporidium (HMSO 1999). Although the data have not explicitly improved public health by a quantifiable reduction in waterborne disease, they have improved the operation of water treatment plants. The monitoring efforts were costly, however the outcomes were positive and indirectly improved public health protection. Furthermore, as the laboratories adhered to proficiency schemes, the data generated are quite valuable for risk assessment activities in other countries.
The principle of “pathogen-free water” and a zero level goal for pathogens has been proposed in the United States and is associated with a level of treatment necessary to achieve minimal or tolerable risk to public health. In 1996, the US EPA implemented the Information Collection Rule (ICR) that employed standardized methods to obtain data on pathogen occurrence across the country. Subsequently, the data revealed the significant problems associated with testing and the interpretation of data obtained from multiple laboratories and sample collection sites (ALLEN et al., 2000).
In 2006, the World Health Organization released new recommendations for the development of drinking water quality guidelines; this report placed an emphasis on the importance of public health outcomes within the context of water monitoring. A monitoring system must be responsive to public need and regulatory mandates, but should not be equated with direct pathogen monitoring. Rather, it should be linked to a health-based target setting that relies on water quality guidelines that are linked to performance measures (indicator monitoring (physical, chemical and microbiological) for process optimization) (WHO, 2006).
In a health-based framework, routine monitoring of source water may be needed to understand the quality of the source water, for an integrated management approach to the watershed and for the optimization of the operation of downstream water treatment plants, often referred to as the ‘source to tap’ approach. Source water analyses may then inform the design of routine monitoring strategies and the optimization of treatment. However, continuous pathogen monitoring of finished water is not considered a feasible or cost-effective solution in this context (WHO, 2006; NHMRC, 2004; CCME, 2004).
Pathogen monitoring of watersheds is also useful for research-driven ecological modelling initiatives. Within the next decade, it is hoped that ecological models will be able to discern, ahead of time, when a particular pathogen will impact the watershed, and subsequently, the water treatment plant. However, in order for the proposed predictive models to be scientifically valid, it is important to critically evaluate the quality of the data used to build the models (GIS data, flow data, climatic data, and microbial monitoring data) (HUNTER, 2003).
In summary, it may be useful to monitor for pathogens in source waters in certain cases, and these initiatives will impact the local level. It is obvious that validated methods are needed, in conjunction with a comparable characterization of the source water. Standardization is a necessity and, in some cases, better detection methods are needed within defined fields of application.
Currently in Canada, there is no documentation (database) of pathogen monitoring initiatives that are ongoing in different watersheds across the country. In addition, the methods used in each of these studies are often not comparable, limiting the usefulness of integrating local data for more comprehensive risk assessment initiatives to inform water safety policy and decision-making. Given the high cost of pathogen testing – and this will probably not change in the near future – is the cost of routine pathogen testing justified? Could a good combination of microbial and non-microbial parameters be a more cost-effective monitoring solution (DUFOUR et al., 2003)? At the very least, developing a mechanism for standardizing monitoring approaches and the subsequent integration of pathogen monitoring data is needed at a national level in Canada. The governmental committees that set drinking water quality guidelines have supported the adoption of a source-to-tap approach, and the integration of local and provincial initiatives would strengthen the quality of outcomes of these investments.
For those that perform the testing and for those that regulate and enforce drinking water regulations across Canada, the need for standardization is imperative. A level of confidence associated with the monitoring of water for non-regulatory initiatives would thus be provided, and a confidence in the data that are produced would be improved. By making a general conclusion through pooling comparable data, the outcome is further justified, especially for watersheds with similar characteristics. Local initiatives could then be compared on a national level.
4. Data for Risk Assessment
Quantitative microbial risk assessment (QMRA) is an emerging field and is rapidly becoming a tool for risk management (FEWTRELL and BARTRAM, 2001; HAAS, 2002; PRUSS et al., 2002). QMRA is a structured, integrative, quantitative and multidisciplinary method to assess microbial risk. It invovles four steps that include: (a) hazard identification, (b) hazard characterization, (c) exposure assessment and (d) risk characterization to inform risk management. It is useful to evaluate interventions, demonstrate the level of consumer protection, and define risk-based criteria for decision-making. One weakness of the QMRA approach is that risks are often associated with peak exposures and not with average exposures. As well, QMRA is supported by data of varying quality.
QMRA is a useful tool to develop criteria for human exposures to pathogens. There is an opportunity to extend the usefulness of this tool in water and other applications, if new information can be obtained to complement existing data, such as the effects of both strain and host differences on the virulence of various pathogens, population level disease dynamics, and the ability of animal data to serve as a predictor of human infectivity.
Researchers must remain vigilant at assessing the value of the models produced in QMRA. For example, in Milwaukee, in 1993, based on current models, the estimated size of 405,000 cases would be expected. However, it would appear that retrospective community-based studies of diarrhoeal disease are subject to recall bias that overestimates the incidence of illness, especially following media reports and public awareness campaigns. It has been suggested that the estimated size of the Milwaukee outbreak is severely flawed, and the actual size of this outbreak was between 1% and 10% of that claimed (HUNTER and SYED, 2001).
Several risk models (HAAS, 2002) have been developed using data from the experimental exposure of volunteers to various pathogens, but it is also possible to use observational data from outbreaks. In both cases, the measurement of the pathogen dose is a prerequisite. The lack of precise detection and enumeration methods has critically limited the value of most of the data obtained. It is not possible to define the dose without the proper metric.
Unlike chemical contaminants, microorganisms pose very different challenges; major differences between strains of the same species can vary greatly in their degree of pathogenicity (HeymanN, 2001). For example, there are numerous strains of E. coli that range from being deadly to exhibiting no pathogenicity — this, however, is not commonly known or understood by many that communicate drinking water microbiology data. Too many scientists that study water as a discipline have little microbiological background and still consider coliforms as pathogens or present microbiological data with a biased perspective.
It is therefore imperative that methods for pathogen detection also include means of estimating the associated virulence. The development of molecular methods is progressing rapidly in this field and in a few years the rapid typing of pathogens should be possible, thereby providing better estimates for risk assessment models (MEDEMA et al., 2003).
In Canada, several groups are investigating waterborne disease risk assessment, including the Canadian Research Institute for Food Safety (http://www.uoguelph.ca/ OAC/CRIFS/), NERAM (http://www.irr-neram.ca/) and the Institute for Population and Public Health (http://www.cihr-irsc.gc.ca/e/institutes/ipph/).
Quantitative risk assessment at this stage has been qualified as being fuzzy and critics point out that there is a great deal of resources spent on risk assessment that is spent unwisely, without a proper evaluation of the quality of the methods or the data outputs. In addition, the current data available on waterborne pathogens are often extremely limited and the concern is that there are people using poor data to fuel various risk assessment approaches without considering the weaknesses associated with the methods. The concern is that decision-making is ahead of the science (PAYMENT and HRUDEY, 2004).
5. Indicators, Pathogens and Disease
Indicators of fecal contamination have served us very well since the early 20th century. Fecal bacteria will always be present when sanitary sewage is discharged in receiving waters. Attempting to correlate the presence of pathogens with fecal indicators is relatively easy when fecal contamination is high. It becomes a probability, not a correlation, at low levels. Pathogens are an inherently moving target as they hit susceptible populations and can almost disappear for months or years. The lack of direct correlation is due to a variety of factors, including the way in which pathogens and indicators are measured, inherent watershed variations, the location of sample collection (water intake – midstream, or recreational samples from beaches), and differences between culture-based and molecular-based identification methods.
In terms of drinking water, treatment selectively removes the less resistant pathogens and indicators but occasionally fails to remove the most resistant ones (MEDEMA et al., 2003).
Microbiological indicators have been, and continue to be, misused; fecal indicator organisms are mainly effective as an indication of fecal contamination, and bacterial indicators such as the thermotolerant coliforms and generic E. coli, do not necessarily correlate directly with the presence or occurrence of pathogens. Their presence is an indication of the potential for pathogen occurrence. Microbiological treatment indicator organisms can provide a measure of removal or inactivation efficiencies of a treatment process. None of the current indicators is a predictor of infection, outbreak or disease (PAYMENT et al., 2003).
Turbidity (a physical indicator) of raw (untreated) water is the only parameter that appears to have some relationship with temporal variations of the incidence of disease in populations (PAYMENT et al., 2003). A 2000 Health Canada study of the Greater Vancouver Regional District (GVRD) identified the link between an increase in endemic waterborne disease and peaks in turbidity, as an indicator of water quality (ARAMINI et al., 2000), providing evidence that during the study period, enteric waterborne pathogens present in each of GVRD’s three drinking water supplies contributed to endemic gastroenteritis among the Greater Vancouver community.
6. Monitoring Protocols
Monitoring is not exempt from the principles of good science, and must be hypothesis driven. Monitoring protocols can be, and should be, very strict. Given the fact that pathogen testing remains expensive, most protocols limit monitoring to a minimal number of samples. The validity of these limited samplings is often questionable given the heterogeneity of pathogens in water.
Water treatment utilities across the country must demonstrate due diligence and meet compliance because of the regulations (especially since post-Walkerton), and that is how the hypothesis is proven (by monitoring). Unfortunately, too many believe that sampling frequency for monitoring could be reduced, rather than expanded, due to associated resource/revenue demands that arise from intensive monitoring efforts. Monitoring drinking water for parameters that result in mainly negative results could be a relatively unwise decision (i.e., coliforms in disinfected water). In fact, if continuous monitoring of treatment through chlorine residual and turbidity levels is performed, the value of bacteriological monitoring is reduced. In-plant microbial reductions can be biologically monitored using HPC values or better aerobic spore-former counts. Distribution system monitoring is still a critical step in the monitoring of treated drinking water and microbial fecal indicators remain the best parameter for this application. Direct pathogen monitoring of treated water does not provide the best cost-benefit solution, given the multitude of pathogens that would need to be analyzed (MEDEMA et al., 2003).
One of the conclusions from the O’Connor report (O’CONNOR, 2002a) was that continuous chlorine monitoring on Well 5 in Walkerton would have prevented the outbreak — this was the only conclusion that used the word «prevent», and it involves a solution that costs a few thousand dollars. This is an important point to consider, when evaluating the true cost of monitoring for pathogens with the optimization of the operation and maintenance of small and large water treatment plants.
7. Methods and Data
Currents methods for the detection of many pathogens are relatively efficient. Methods for viruses and parasites can easily detect as few as one microorganism per 1,000 litres with very good efficiency of 20 to 50% (PAYMENT et al., 2000; PAYMENT, 2002). They suffer, however, because they are considered expensive (untrue relative to many chemical analyses), require trained personnel (true for many tests, including chemical analyses), require biosafety precautions (a true risk) and do not provide timely results (true for most methods, but are faster results needed).
Molecular methods may provide better sensitivity, but at the cost of losing answers that address the viability and infectivity of the detected pathogens. A combination of culture methods and molecular methods provides greater sensitivity for pathogens that can be cultivated (MEDEMA et al., 2003; PAYMENT and RILEY, 2002)).
In addressing the issue of methodology, the assumption is that there should be no pathogens in treated drinking water, during the proper operation of a water treatment plant. In order to provide that level of information, current methods fall short. Thus, new methods are needed to attempt to answer these questions — very sensitive methods that have been validated, to determine if indicators and/or pathogens are present in treated water, whether the pathogens are infective and their potential to cause disease in the human population.
Data on the occurrence of pathogens in water are not comparable, given the number of differences in methodologies (ANON, 1999). They are therefore difficult to share and exchange unless the caveats of the methods are carefully weighted.
New methods for detecting waterborne pathogens remain in the developmental stage. In particular, their sensitivity must be improved, mainly because of the challenge of detecting low level of pathogens in water: large volumes need to be analyzed and most detection methods can only effectively process small volumes. Only a few of the many possible pathogens are currently detectable and, given that water may contain hundreds of different pathogens over time, it is still unclear which pathogens should be detected. Pathogen testing methods are very specific and they do not detect all pathogens present. According to OECD (MEDEMA et al., 2003), molecular methods, coupled with high throughput parallel processing and bioinformatics, hold the promise of detecting a wider range of microorganisms, but are not yet practical. (KÖSTER et al., 2003).
The analysis of water samples for pathogens requires a specialized laboratory, highly trained personnel and appropriate bio-safety containment (PAYMENT, 2001; PAYMENT, 2002; HURST et al., 2002; APHA et al., 1998). In industrialized countries, few laboratories outside the clinical setting meet these requirements, and in many other countries, such facilities do not exist. Pathogen testing may require the growth and manipulation of pathogens, thus the potential risk to analysts needs to be considered. Although some pathogens can be detected rapidly, most pathogen sampling and detection methods still have a time-to-verified-result of several days. Pathogen testing of treated water does not escape the problems identified with end-product testing using traditional bacterial parameters, i.e. they signal that something is wrong after the problem has occurred. These methodological limitations advocate the use of great care in the interpretation of results from pathogen testing. Any positive result may indicate that water is unsafe to drink and can be used to estimate the level of risk to consumers. Positive results should be used only in a well-managed, risk-based decision-making process. Negative results should always be viewed with some scepticism, given the large number of possible pathogens that could be present, and should not be used as an excuse for complacency (HRUDEY and RIZAK, 2004).
Again, according to OECD (MEDEMA et al., 2003), the challenges that remain for the development of new pathogen detection methods are:
Quantification – The quantitative aspects need to be improved as current molecular methods are, at best, only semi-quantitative.
Infectivity – The viability and infectivity of the detected microorganisms is still uncertain.
Concentration – Detection of (especially pathogenic) microorganisms in water requires assaying large volumes (0.1-100 litres or more), while the new technologies currently work with small volumes (0.00001-0.001 litres). This requires concentration methods that introduce recovery losses.
Skills and novel infrastructure (both in personnel training and equipment) – Further implementation of these technologies in practice ideally requires further simplification and also automation.
Cost – The cost is still high and currently not amenable to frequent daily testing within the budget constraints of small water suppliers.
8. Laboratory Capacity
Contrary to the United States, but not different from most other countries, few laboratories in Canada possess the capability to analysz environmental samples for the wide range of potential waterborne pathogens. Some have developed bacteriological expertise and few have parasitological or virological expertise. There are many commercial laboratories with accreditation by CAEAL (Canadian Association for Environmental Analytical Laboratories) or by local provincial authorities; although they typically specialize in routine analysis for parameters that are specified by current drinking water regulations (coliforms and generic E. coli). This means that pathogens are not on their list of offered services. Although several university labs in Canada can perform some pathogen testing, most do not adhere to an accredited QA/QC quality system and do not meet basic Good Laboratory Practices (GLP) standards. There is therefore no system, at the academic level, to validate the results that are published in peer-reviewed literature and subsequently interpreted by industry and the research community.
In some Canadian provinces, it appears that post-Walkerton regulations have decreased the already frail pathogen testing capacity, stalling the process as test method development is hindered by validation/licensing requirements by the provincial government. However, the benefits associated with more stringent regulations include preventing laboratories from performing tests and methods that they do not have the capacity or skill to perform adequately. Additionally, Ontario is in the process of developing legislation that embraces the HACCP ‘source-to-tap’ approach to source protection, addressing all sources of drinking water at the watershed level, in response to the O’Connor recommendations (MOE, 2004). Source protection plans will be prepared by local source protection committees within each watershed, with involvement and input from all levels of government as well as local communities and stakeholders. The source protection committees will identify the risks (significant, moderate, and low) of contamination or depletion to their drinking water sources, and identify actions to reduce those risks (MOE, 2004). It is still unclear how pathogen monitoring will be integrated into these plans.
Data on waterborne pathogens are being generated and used across the country. However, it is still unclear whether the benefits of waterborne pathogen testing outweigh the costs, especially if the current methods are not adequately sensitive or specific and are poorly controlled. No current waterborne pathogen monitoring method has the capability of providing results of adequate sensitivity, specificity or reproducibility for the protection of public health (ALLEN et al., 2000).
Routine pathogen monitoring of drinking water is probably not the solution, given that well-operated treatment systems should provide almost full removal and/or inactivation of pathogens, eliminating the value of testing for pathogens with expected negative results. Monitoring for specific pathogens in raw (untreated) water can provide a basis for quantitative risk assessments at the local level, but these activities should be performed within the context of a watershed management framework that incorporates all stakeholders in the process, including the local government offices (environment, agriculture, health), conservation authorities, public health unit, and water utility.
There are benefits to having enhanced pathogen detection methods performed by accredited laboratories and investing in laboratory capacity to develop, adopt, and standardize traditional and new approaches: in an outbreak situation, there is a critical need for enhanced laboratory capacity to identify pathogens and inform the epidemiological decision-making of outbreak investigations.
9. Education and Communication
The differences between pathogens and indicators, and their usefulness in water monitoring and the provision of safe drinking water must be clarified. Too many still have a preconceived (and false) understanding of the issues related to water microbiology.
Risk communication related to microbial data is also needed. Rather, if the quality of the monitoring data is ambiguous, then the true public health risks are still unknown, and very difficult to accurately communicate, both within the discipline and to the general public. There are a number of people that are tasked with communicating public health risks associated with waterborne pathogens that they do not fully understand the issues. This potentially leads to misinformation and sensationalization of the information, by not placing the microbial data in the proper context.
The topic is complex and multifaceted, but “seeing is believing”. How many children have looked at pond water through a microscope? One can’t help but believe it is complex if the issue is presented with that image.
Those delivering the message and those hearing the message need to understand that microorganisms are ubiquitous, few are dangerous, and there are difficulties related to the detection of microorganisms that still need to be overcome. Furthermore, it is important to convey the message that a negative result should not imply complacency or zero-risk, while a positive result should not always imply a public health risk or emergency.
The general public, scientific, government, regulatory and utility communities at large, and the international community need to better understand the scope of the issues discussed herein, in order to accurately manage public response to emerging drinking water safety and public health issues (O’CONNOR, 2002b; PAYMENT and RILEY, 2002).
10. Conclusion
Current and future research must address the issues of methodology, sensitivity, specificity, and negative and positive predictive values related to the detection of pathogens if they hope to impact the delivery of safe drinking water to communities in Canada. Recent findings suggest that there are large errors associated with the predictive value of mostly negative results (HRUDEY and LEISS, 2003; HRUDEY and RIZAK, 2004). Microbial drinking water safety research must be purpose-driven, with a public health perspective, in order to better understand the source of waterborne pathogen transmission, and inform public health priority decision making at the regional, provincial and national levels.
In summary, a systems approach is needed to address this issue. It is no longer adequate to simply focus on pathogens. Protection of source water and an HACCP or multi-barrier approach (http://www.hc-sc.gc.ca/hecs-sesc/water/index.htm) should provide solutions within the context of delivering public health protection (WHO, 2004).
“Individual treatment for every parameter and pathogen is not possible. As a result, drinking water risk management has needed some refocusing and a trend has emerged back towards emphasizing good practice and achieving effective, multiple barriers to assure drinking water safety rather than a narrow focus strictly on achieving numerical guideline targets.” (FAZIL et al., 2003).
Parties annexes
Acknowledgements
This paper is based on a mini-colloquium entitled “Waterborne Pathogens in Canada: a Critical Assessment of Methods and Test Results”, sponsored by the Canadian Water Network and held April 3, 2004 in Calgary, Alberta, Canada. The authors express their sincere thanks to the following participants who contributed their expertise and knowledge: Jim Byrne (University of Lethbridge, Lethbridge, Alberta), Bernadette Conant (Executive Director, Canadian Water Network, Waterloo, Ontario), Les Gammie (EPCOR, Edmonton, Alberta), Victor Gannon (Health Canada, Lethbridge, Alberta), Peter Huck (University of Waterloo, Waterloo, Ontario), Judy Isaac-Renton (Director, BC CDC Laboratory, Vancouver, British Columbia), Cassandra Lafranco (Senior Microbiology Advisor, Ministry of Environment, Toronto Ontario), Gary Palmateer (Director, GAP EnviroMicrobial Services Inc., London, Ontario), Donald Reid (Scottish Executive, Scotland, UK), Will Robertson (Health Canada, Ottawa, Ontario), Susan Springthorpe (Director of Research, Centre for Research on Environmental Microbiology (CREM), University of Ottawa, Ottawa, Ontario), Mark Servos (Director, Canadian Water Network, Waterloo, Ontario).
References
- ALLEN M.J., CLANCY J.L. and E.W. RICE, 2000. The plain, hard truth about pathogen monitoring. JAWWA, 92, 64-76.
- ANON, 1999. Waterborne pathogens. AWWA Manual of Water Practices, M48. American Water Works Association, Denver, Colorado.
- ARAMINI J., McLEAN M., WILSON J., HOLT J., COPES R., ALLEN B. and W. SEARS, 2000. Drinking water quality and health-care utilization for gastrointestinal illness in greater Vancouver. Can. Commun. Dis. Rep. (CCDR), 26, 212-214. (Complete report: www.hc-sc.gc.ca/ehp/ehd/catalogue/bch_pubs/vancouver_dwq.htm).
- APHA, AWWA, WEF, 1998. Standard methods for the examination of water and wastewater (20th Edition). CLESCERI L.S., GREENBERG A.E. and EATON A.D. (Editors). Published by the American Public Health Association, the American Water Works Association and the Water Environment Federation, Washington DC, USA.
- BATZ M.B., DOYLE M.P., MORRIS J.G. Jr, PAINTER J., SINGH R. and R.V. TAUXE, 2005. Attributing illness to food. Emerg Infect Dis., 1, 993-999.
- CCME, 2004. Source to tap: guidance on the multi-barrier approach to safe drinking water. Federal-Provincial-Territorial Committee on Drinking Water and Canadian Council of Ministers of the Environment, ISBN 1-896997-48-1.
- COLFORD J.M., WADE T.J., SANDHU S.K, WRIGHT C.C., LEE S., SHAW S., FOX K., BURNS S., BENKER A., BROOKHART M.A., VAN DER LAAN M. and D.A. LEVY, 2005. A randomized, controlled trial of in-home drinking water intervention to reduce gastrointestinal illness. Am. J. Epid., 161, 472-482.
- CRAUN G.F., 1992. Waterborne disease outbreaks in the United States of America: causes and prevention. World Health Stat. Q. 45,192-9.
- DUFOUR A., SNOZZI M., KÖSTER W., BARTRAM J., RONCHI E. and L. FEWTRELL, 2003. Assessing microbial safety of drinking water: improving approaches and methods. WHO Drinking Water Quality Series, OECD – WHO, Paris, France (IWA Publishing, London).
- FAZIL A., PAOLI G., LAMMERDING A., DAVIDSON V., S. HRUDEY, ISAAC-RENTON J. and M. GRIFFITHS, 2003. Needs, gaps and opportunities assessment (NGOA) for microbial risk assessment in food and water. Canadian Research Institute for Food Safety, Guelph (Ontario), Canada, 76 p. (http://www.uoguelph.ca/crifs/NGOA/ Finalupdates/NGOAfinalreport.pdf).
- FEWTRELL L. and J. BARTRAM, 2001. Water quality: Guidelines, standards and health. Assessment of risk and risk management for water-related infectious disease. IWA Publishing, London, UK., 424 p.
- FROST F.J., KUNDE T.R. and G.F. CRAUN, 2002. Is contaminated groundwater an important cause of viral gastroenteritis in the United States? Environ. Health, 65, 9-14.
- HAAS C.N., 2002. Progress and data gaps in quantitative microbial risk assessment. Water Sci. Technol., 46, 277-284.
- HALD T., VOSE D., WEGENER H.C. and T. KOUPEEV, 2004. A bayesian approach to quantify the contribution of animal-food sources to human salmonellosis. Risk. Anal., 24, 255-269.
- HELLARD M.E., SINCLAIR M.I., FORBES A.B. and C.K. FAIRLEY, 2001. A randomized, blinded, controlled trial investigating the gastrointestinal health effects of drinking water quality. Environ. Health Perspect., 109, 773-778.
- HEYMANN D.L., 2001. Control of communicable diseases manual. 18th Ed. American Public Health Association, Washington, DC 20001, USA.
- HMSO, 1999. The water supply (water quality) (amendment) regulations 1999, Statutory instrument 1999, No. 1524. Her Majesty’s Stationery Office, London.
- HRUDEY S.E. and E.J. HRUDEY,, 2004. Safe drinking water: Lessons from recent outbreaks in affluent nations. IWA Publishing, Cornwall, United Kingdom, 486 p.
- HRUDEY S.E. and S. RIZAK, 2004. Discussion of rapid analytical techniques for drinking water security investigations. JAWWA, 96, 110-113.
- HRUDEY S.E. and W. LEISS, 2003. Risk management and precaution – insights on the cautious use of evidence. Environ. Health Perspect., 111, 1577-1581.
- HUNTER P.R., 2003. Climate change and waterborne and vector-borne disease. J. Appl. Microbiol., 94, 37S-46S.
- HUNTER P.R. and Q. SYED, 2001. Community surveys of self-reported diarrhoea can dramatically overestimate the size of outbreaks of waterborne cryptosporidiosis. Water Sci. Technol., 43, 27-30.
- HUNTER P.R. and L. FEWTRELL, 2001. Acceptable risk. In: Water Quality: Guidelines, Standards and Health. Assessment of risk and risk management for water-related infectious disease. DUFOUR A. et al. (Editors.), IWA Publishing, London, 207-227.
- HUNTER P.R., 1997. Waterborne disease. Epidemiology and ecology. John Wiley and Sons, Chichester, United Kingdom, 372 p.
- HURST C.J., KNUDSEN G.R., MCINERNEY M.J., STETZENBACK L.D. and R.L. CRAWFORD, (Editors), 2002. Manual of environmental microbiology, 2nd edition, ASM Press, Washington, DC, USA.
- KÖSTER W., EGLI T., ASHBOLT N., BOTZENHART K., BURLION N., ENDO T., GRIMONT P., GUILLOT E., MABILAT C., NEWPORT L., NIEMI M., PAYMENT P., PRESCOTT A., RENAUD P. and A. RUST, 2003. Analytical methods for microbiological water quality testing. In: Assessing microbial safety of drinking water: Improving approaches and methods. DUFOUR A. et al. (Editors), WHO Drinking Water Quality Series, OECD – WHO, Paris, France (IWA Publishing, London), 237-295.
- KUUSI M., AAVITSLAND P., GRONDROSEN B. and G. KAPPERUD, 2003. Incidence of gastroenteritis in Norway - a population-based survey. Epidemiol. Infect., 131, 591-597.
- LEE M., 2003. Enteric illness in Ontario, Canada, from 1997-2001. Public Health and Epidemiology Report Ontario, 14, 175-186.
- LEE S.H., LEVY D.A., CRAUN G.F., BEACH M.J. and R.L. CALDERON, 2002. Surveillance for waterborne-disease outbreaks-United States, 1999-2000. Surveillance Summaries, MMWR, 51, SS-8, 1-48.
- MAJOWICZ S.E., DORE K., FLINT J.A., EDGE V.L., READ S., BUFFETT M.C., McEWEN S., McNAB W.B., STACEY D., SOCKETT P. and J.B. WILSON, 2004. Magnitude and distribution of acute, self-reported gastrointestinal illness in a Canadian community. Epidemiol. Infect., 132, 607-617.
- MEDEMA G.J., PAYMENT P., DUFOUR A., ROBERTSON W., WAITE M., HUNTER P., KIRBY R. and Y. ANDERSSON, 2003. Safe drinking water: an ongoing challenge. In: Assessing microbial safety of drinking water: Improving approaches and methods. DUFOUR A. et al. (Editors), WHO Drinking Water Quality Series, OECD – WHO, Paris, France (IWA Publishing, London), Chapter 1.
- MOE (MINISTRY OF ENVIRONMENT), 2004. Watershed-based source protection: implementation committee report to the Minister of the Environment, November 2004. Queen’s Printer of Ontario, PIBs 4938e.
- NHMRC, 2004. Australian drinking water guidelines, National Health and Medical Research Council, Australian Government, ISBN 1864961244.
- O’CONNOR D.R., 2002a. Report of the Walkerton inquiry: Part 1 – The events of May 2000 and related issues. The Walkerton Inquiry, Toronto, 504 p.
- O’CONNOR D.R., 2002b. Report of the Walkerton inquiry: Part 2 – A strategy for safe drinking water. The Walkerton Inquiry, Toronto, 588 p.
- PAYMENT P. and S.E. HRUDEY, 2004. Is drinking water quality management in Canada based on health risk? Proceedings of the 11th National Conference on Drinking Water, Calgary, Alberta, April 3-6, 2004.
- PAYMENT P., WAITE M. and A. DUFOUR, 2003. Introducing parameters for the assessment of drinking water quality. In: Assessing microbial safety of drinking water: Improving approaches and methods. DUFOUR A. et al. (Editors) WHO Drinking Water Quality Series, OECD – WHO, Paris, France (IWA Publishing, London), 47-77.
- PAYMENT P. , 2002. Cultivation of viruses from environmental samples. In: Manual of Environmental Microbiology, 2nd edition. Hurst C.J.et al. (Editors), ASM Press, Washington DC, USA, 84-91.
- PAYMENT P. and M. RILEY, 2002. Resolving the global burden of gastrointestinal illness: a call to action. American Academy of Microbiology, Washington, DC, 26 p.
- PAYMENT P. and P.R. HUNTER, 2001. Endemic and epidemic infectious intestinal disease and its relationship to drinking water. In: Assessing microbial safety of drinking water: Improving approaches and methods. DUFOUR A. et al. (Editors) WHO Drinking Water Quality Series, OECD – WHO, Paris, France (IWA Publishing, London).
- PAYMENT P., BERTE A., PRÉVOST M., MÉNARD B and B. BARBEAU, 2000. Occurrence of pathogenic microorganisms in the Saint-Lawrence river (Canada) and comparison of health risks for populations using it as their source of drinking water. Can. J. Microbiol., 46, 565-576.
- PAYMENT P., SIEMIATYCKI J., RICHARDSON L., RENAUD G., FRANCO E. and M. PRÉVOST, 1997. A prospective epidemiological study of gastrointestinal health effects due to the consumption of drinking water. Int. J. Environ. Health Res., 7, 5-31.
- PRÜSS A., KAY D., FEWTRELL L. and J. BARTRAM,, 2002. Estimating the burden of disease due to water, sanitation and hygiene at global level. Environ. Health Perspect., 110, 537-42.
- SAID B., WRIGHT F., NICHOLS G.L., REACHER M. and M. RUTTER, 2003. Outbreaks of infectious disease associated with private drinking water supplies in England and Wales 1970-2002. Epidemiol. Infect., 130, 469-479.
- SCALLAN E., FITZGERALD M., COLLINS C., CROWLEY D., DALY L., DEVINE M., IGOE D., QUIGLEY T., ROBINSON T. and B. SMYTH, 2004. Acute gastroenteritis in northern Ireland and the Republic of Ireland: a telephone survey. Commun. Dis. Public Health, 7, 61-67.
- US ENVIRONMENTAL PROTECTION AGENCY, 2003. National primary drinking water regulations: Long term enhanced surface water treatment rule. US Federal Register 68, 154. (Monday, August 11, 2003), 47640-47795.
- WHEELER J.G., SETHI D., COWDEN J.M., WALL P.G., RODRIGUES L.C., THOMKINS D.S., HUDSON M.J. and P.J. RODERICK, 1999. Study of infectious intestinal disease in England: rates in the community, presenting to general practice, and reported to national surveillance. The Infectious Intestinal Disease Study Executive. British Med. J., 318, 1046-1055.
- WHO, 2003a. Emerging issues in water and infectious disease. World Health Organization, Geneva, 24 p. Available on-line: www.who.int/ water_sanitation_health/emerging/emergingissues/en/.
- WHO, 2003b. The World Health Report: Chapter 5: SARS lessons from a new disease. World Health Organization, Geneva.
- WHO, 2006. WHO guidelines for drinking water quality, 3rd (current) edition, including the first addendum. Volume 1. Recommendations. World Health Organization, Geneva, 515 p.
Liste des tableaux
Table 1
Diseases, agents and symptoms associated with waterborne disease (data from HeymanN 2001).
Maladies, microorganismes et symptômes associés aux maladies transmises par la voie hydrique (données modifiées de Heyman 2001).
Table 2
Diseases and syndromes associated with enteric viruses.
Maladies et syndromes associés aux virus entériques.